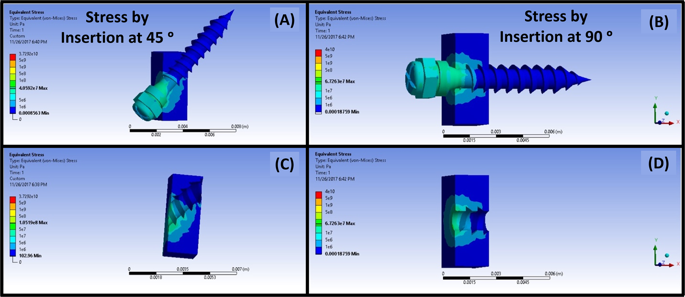
The process of microimplant insertion into cortical bone leads to the generation of stresses in the cortical bone. Accumulation of stress in the cortical bone leads to formation of microdamage of the cortical bone as a method to relieve the stresses accumulating around the microimplant. The occurring microdamage can present itself as distinct or diffuse microcracks, as micro elevation of the cortical bone relative to microimplant placement and by formation of bone debris due to the screwing motion of the microimplant as it drills through the bone structure. To attain a more extensive picture of the accumulation of the stress, we ran a simulation of microimplant placement using the FEA method in two different angulations. As per the result of the simulation, we could concur that majority of the von misses stresses that were generated were at the subsurface level of the cortical bone in both the angulations and at the obtuse angle created between the microimplant and the bone surface. With this information in hand we then proceeded to the experiment phase of the research protocol.
As we could understand from the previous literature of OCT systems, we needed to remove any bias pertaining to the reflectivity of light, as it bounces of the metal surface of the microimplant and projects as a microcrack, leading us to a false positive result. Thus, we initially used a pilot drill to create holes on the bone surface at two different angulations and determined the presence of microdamage formation by scanning the pilot drill hole with the OCT system. The results of which are shown in Fig. 2.
After the scanning process, the image generated were transferred onto a volumetric software and processed. The image is projected into a series of images, each making up an individual slice of the compete image. For the purposes of removing any bias, to avoid false positive results and for facile reproduction of the results, we defined the microdamage to be; (a) microcrack, i.e., seen as a clear and distinct discontinuation of the cortical bone emanating from and around the microimplant surface. To be classified a microcrack, the actual crack needed to be present in 5 or more consecutive OCT images lateral and in the depth direction. (b) micro-elevation and (c) bone debris formation. Furthermore, we confirmed our findings with the use of micro-computed tomography, the scanning modality that is considered to be a gold standard in hard tissue imaging to determine the presence of microcracks in the cortical bone around the microimplant surface.
From the data presented in the study, we can derive OCT to be an effective tool to be used as a non-invasive imaging modality to detect and asses cortical bone microdamage occurring around the microimplant bone interface and the obtained images can be processed and analyzed to study the entities in a 3-dimensional manner.
Freshly extracted bovine bone samples were initially scanned to set a base line for the study. Following which, pre-microimplant holes were drilled and the samples were scanned. The samples were divided into four groups of 20 microimplants each and the microimplants were inserted onto the bone samples as prescribed by the manufacturer. After loading of the microimplants into the bone samples, individual samples were scanned using the OCT systems. With the use of our OCT system, we could achieve a depth of 250 μm into the cortical bone and this depth coincides with the high stress patterns previously shown in our FEA model. Even though, the penetration of the OCT system is not sufficient to image the micro-implant through its entirety, it provides images of adequate penetration depth and high resolution of the surface of the cortical bone.
As shown in Fig. 3, the areas of microdamage around the microimplant-bone interface are clearly visible in the OCT images. Microdamage, as defined, is the combination of microcracks, micro elevation and bone debris formation, collectively effecting the structural integrity of the cortical bone around the microimplant and in OCT images is seen as areas of different intensity and elevations on different planes as compared to the surrounding normal bone surface. These affected areas are seen around the implant surface and propagate to an area of up to 1 mm.
Depth intensity profile analysis was performed using Matlab coding, to confirm and evaluate the presence of micro cracks around the bone-implant interface. The sudden drop in the intensity corresponds to the discontinuity in the bone structure around the implant, validating the visualization of micro cracks present in the 3D model. This feature of OCT sets it apart from other commonly used imaging modality, as quantitative analysis pertaining to the nature of the micro crack can be obtained. In the following study, Fig. 4 represents the depth intensity profile analysis of the obtained OCT images. Following the depth intensity profile analysis, the results of the quantitative analysis of the occurring microdamage is tabulated in Table 1 as shown.
Area of microdamage cover is noted to be more when microimplants are placed in the no-drilling method and visibly lower when a pre-drill hole is made prior to the microimplant insertion. This could be due to the additional torque that needs to be generated whilst placement of the microimplant in the no-drill method. Additionally, when the microimplant is placed at an angle of 45° in both the insertion methods, the occurring microdamage is increased, owing to the fact that when we place the microimplant at an angle, there is more engagement of the cortical bone with the microimplant leading to increased insertion torque and subsequently increased microdamage23.
Primary stability of the microimplant is a determining factor for the success of the microimplant. Quality of the bone structure is a vital aspect of primary stability, and the occurring bone microdamage can directly affect the stability of the microimplant. As observed in Figs 3 and 4, microcracks can be visualized as minute discontinuity of the cortical bone around the implant. Numerous microcracks are present, but only a few large microcracks are seen navigating around the mini-screw implant. Primary stability of the implant depends on the inter-locking mechanism between the mini-screw implant the bone surrounding the implant. During the process of insertion, the torque generated can lead to the formation and propagation of microcracks through the bone structure24,25. Microcracks can cause a significance effect to the primary stability of the implant. Large microcracks can develop into areas of weak bone structure and compromise the balance at the bone-implant interface, leading to failure of microimplants26. In our study, we noticed the presence of microcracks all around the implant, especially correlating with the direction of placement of the microimplants and the method of microimplant placement. An increase in the number of cracks was noticed corresponding to the angulation of mini-screw implant placement and the mode of microimplant placement. When the implant was placed at an angle of 45°, an increase in number of microcracks was seen, as when compare with 90° angle placement. This could be due to the fact that, when placed at an angle of 45°, the implant transverses more on the cortical bone as compared to 90° angulation27. Operator dexterity and precision during application of force whilst implant placement can be a reason for the occurrence of microcracks on the bone structure. High resolution and high contrast images generated by OCT, benefits the visualization of the microcracks around the bone-implant interface. Furthermore, utilizing the 3D scans, a comprehensive analysis of the microcracks direction and means of propagation can be attained using OCT technique.
Micro elevation is another important aspect effecting the primary stability of the microimplant. Angular placement of the microimplant, causes the microimplant to transverse more in the denser cortical bone. As when the threads of the microimplant engages the dense cortical bone, the bone material is pushed upwards as the microimplants transverses forward, leading to areas of micro elevation of the cortical bone, at the superior angle formed between the microimplant and bone surface. These areas as shown in Fig. 5, act as areas of demineralization around the microimplant and can affect the primary stability of the microimplant.
Accumulation of bone debris along the surface of the bone adjacent to the microimplants is of note (Fig. 6). Presence of the bone debris, its shape and quantity are easily evaluated though OCT imaging. In en face images rendered from 3D volumetric OCT images (Fig. 6(B–F)), bone debris can be observed. Bone debris, in the images is seen as large masses of opaque intensities accumulating around the implant head. The presence of these bone debris is due to the non-drilling nature of the microimplants and do not pose a threat to visualize the microcracks on the scanned images. Although, we would advise cautious removal of these debris for better evaluation of the surface underneath the debris. Depth penetration ability of OCT is of added value in relation to the visualization of micro-damage and microcracks on the bone structures, as using the 3D modes, we can navigate through sections underneath the debris to locate and analyze these structures. However, from a clinical point of view, the accumulation of the bony debris adjacent to the microimplant and within the screw threads can lead to an increase of stress within the cortical bone leading to disruptions on the implant-bone interface26.
We confirmed the results of our study, via the means of micro-computed tomography. Micro computed tomography, of late is considered the gold standard for assessing bone morphology and microstructures28. As seen in OCT images, the areas of microdamage is distinctly and more accurately seen in MICRO-CT images, but, the radiation exposure associated with micro-CT is very high. The ionizing effects of the radiation can have an effect on samples. Secondly, the micro-CT imaging technique is relying on the contrast, brightness and signal to noise ration. These parameters are sensitive and can lead to alterations in the image quality. Some imaging artefacts are peculiar to CT, such as ring artefacts and beam hardening and can affect the overall quality of the image.
From a clinical point of view, the prevalence of microdamage, plays a significant role in the primary stability of the microimplant. As seen in our study, placement of non-drilling microimplants at an angle of 45°, caused the maximum damage to the cortical bone. In these cases, the failure rate of microimplant will be increased. Alternatively, we notice minimal microdamage to the cortical bone when the microimplant is placed more perpendicular to the bone surface and when a pre-drill hole is placed before the insertion of the microimplant. We can concur that placement of microimplants more perpendicular to the bone surface and by utilization of a pre-drill hole is a better modality for the success of microimplants.
The most important feature of primary stability of microimplants is represented by the intimate contact between the implant and the bone. To investigate such aspects, it is essential to have a noninvasive method to predict the stability of the inserted implants. To this goal, the OCT method could operate non- invasively and allow the orthodontists to evaluate the success and to predict the efficiency of the orthodontic microimplant treatment. The usual investigative methods known such as histological studies and computed tomography are invasive and they exhibit inferior resolution and contrast as compared to OCT imaging. This added information, can contribute to a better prognosis of orthodontic treatment.