All 63 surveys were completed and returned. All had over 90% answers completed and were deemed satisfactory to include for analysis. Most questions had 100% responders, several had 1-3 missing data; only the question “How confident are you in your ability to examine if patient experiences dysphagia?” had 19 nil responses.
Demographics
All participants were female. Most were experienced with clinical experience ≥6years (69.8%, n = 44). Over half had ≥6years of specific experience in pediatric oncology (54.0%, n = 34). The majority were Staff Nurse grade and above; over half were either Senior Staff Nurse or Assistant Nurse Clinician (58.7%, n = 37). Over three-quarters had Bachelor of Nursing degrees (76.2%, n = 48) from countries such as Singapore, Philippines and India. Many did not have oral health-related training (58.7%, n = 37), clinical competency during nursing training (76.7%, n = 46), or Continuing Professional Education (CPE) related to oral health in past 5 years (68.3%, n = 41) (Details: Supplemental Table S1).
Knowledge
No participant answered all knowledge questions correctly. Four (6.3%) had over 90% of questions correct (13 questions); 11 (17.4%) had more than 80% of questions correct (≥12 questions). The majority (92.1%, n = 58) did not know of any local or international guidelines on oral healthcare in pediatric oncology patients.
All participants knew that children undergoing cancer therapy can potentially develop oral complications, and that good oral hygiene is important to reduce the severity of oral mucositis. All but one (98.5%) responded correctly that caregivers should assess patients’ mouth every day during active cancer therapy. Three-quarters (75.8%, n = 47) knew that oral cavity is the most common source of sepsis in immunocompromised patients with cancer. The majority knew the best timing to refer patients is before cancer treatment (81.0%, n = 51).
The majority knew that patients should brush at least twice daily with a soft toothbrush (98.4%, n = 62), regardless of their red blood cell (87.1%, n = 54), or white blood cell levels (83.9%, n = 52). However, half (52.4% n = 33) were mistaken that toothbrushing should not continue if platelet counts are low. Moreover, not all (72.6%, n = 45) knew that a fluoride toothpaste should be used. Approximately half (55.6%, n = 35) knew that oral swabs should not be used for oral hygiene as a long-term substitute for toothbrushing.
Knowledge regarding dietary practices were poor. Only 37.1% (n = 23) knew that frequency of sugary intake is a greater risk factor for dental caries than total amount of sugary intake. Although upward trends in the overall knowledge scores were observed in nurses regardless of their specialty, after attending up to 3 hours of Continuing Professional Education (CPE) related to oral care (Table 2), this did not reach statistical significance.
Attitudes and Beliefs
All participants believed that oral hygiene is important. The majority felt they play an important role in maintaining patients’ oral health (93.7%, n = 59) and ensuring patients brush teeth at least twice daily (95.1%, n = 58). In fact, 92% (n = 57) felt it was “very or somewhat important” to help brush the child’s teeth, if the parents/patients do not do so. However, three-quarters (75.8%, n = 47) felt they needed further training in oral hygiene education.
Perceived Practices
The nurses reflected that it was mostly doctors (85.7%, n = 54) who referred patients to dentists. Moreover, only 61.9% (n = 39) were aware of an existing in-hospital dental referral form.
The majority would check patients’ mouths at least once daily (74.6%, n = 47) (Fig. 1). Oral conditions evaluated most commonly were: oral mucositis (98.4%, n = 62), oral ulcerations (87.3%, n = 55), oral bleeding (85.7%, n = 54), swollen gums (79.4%, n = 50), and oral pain (79.4%, n = 50). Dental caries, inflamed soft tissues, dysphagia, fungal infection, clinical abscess, dental plaque, bad breath, and oral pathology were less frequently evaluated (Details: Supplemental Table S2).
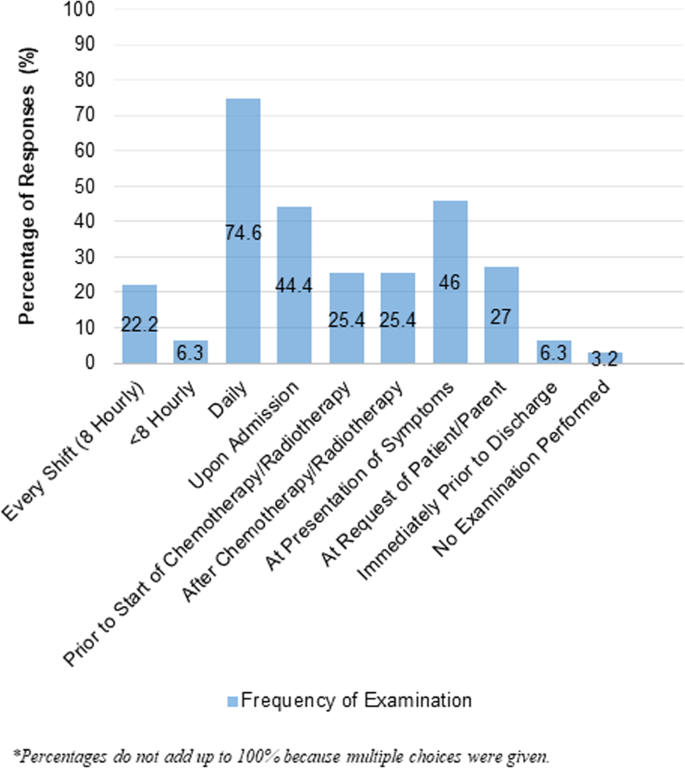
Frequency of oral examination by nurses.
Concerning toothbrushing, 85.7% (n = 54) advised patients to do so “often”/“always”; the rest “seldom”/“never did so”. Only 65% (n = 41) assisted patients to brush their teeth “often”/“always”; the rest “seldom did so”. About three-quarters would recommend fluoride toothpaste (74.2%, n = 46), 9.7% (n = 6) advised non-fluoridated toothpastes, and the rest were “not sure”/”did not” give advice (16.1% n = 10). Common oral health aids advised were foam brush, soft-bristled toothbrush, mouthwash, and lip balm (Details: Supplemental Fig. S1). About half (51.7%, n = 32) advised patients to reduce sugary intake “often”/“always”; the rest “seldom” or “never did so”.
Perceived abilities
The majority felt comfortable (92.1% n = 58), and adequately trained (90.5%, n = 57) performing oral care, including assisting with toothbrushing, mouthwash use, and application of oral topical medications.
Over 80-90% were confident to examine for the health of teeth/gums, presence of oral pathology and oral pain, and discuss importance of regular professional dental care. Over 70-80% were confident to examine for presence of tooth decay, oral appliances or dry mouth, and providing parents with oral hygiene home care and dietary advice to prevent decay. However, only 57.1% (n = 36) were confident in advising fluoride toothpaste use. Likewise, just over 60% were confident in identifying specific problems like trismus and dysphagia (Fig. 2).
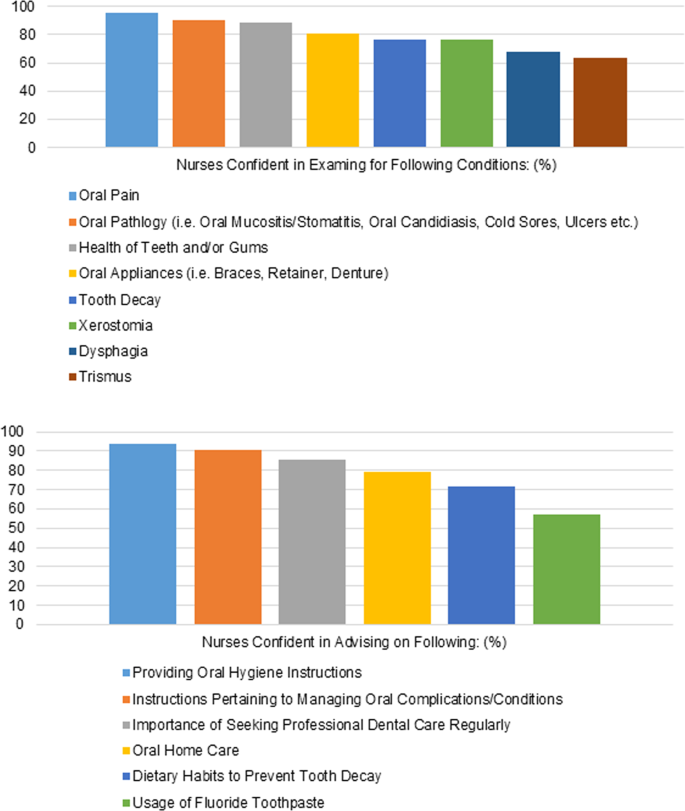
a Confidence in examination of oral conditions. b Confidence in advising parents on oral care of child.
Only 65.1% (n = 41) felt adequately trained to give oral care instructions. Just over half (57.1%, n = 36) felt adequately trained to perform oral examinations.
Barriers
The most common barriers to dental referral reported were beliefs that it is not their responsibility or authority, followed by inadequate knowledge of dental conditions to refer for (Fig. 3).
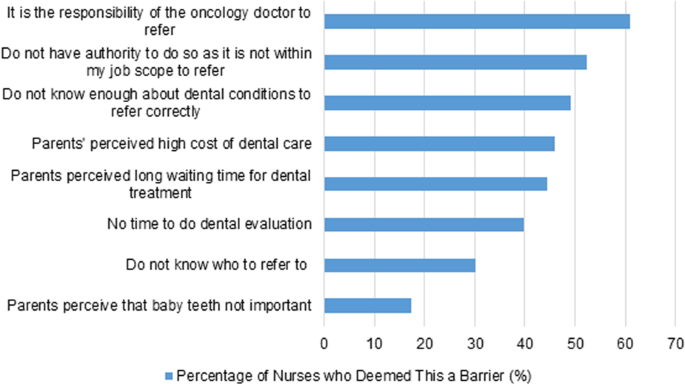
Responses to “Concerns preventing you from referring your patients to see a dentist”.
In terms of barriers to performing oral care, the most common theme was patient-related e.g. poor patient cooperation, patient being unwell or having sore mouth. This was followed by staff and operational factors e.g. inadequate time, staff knowledge, skills, and oral care resources in ward. Most did not find oral care an unpleasant task (90.5%, n = 57) but 42.9% (n = 27) felt it was parents’ responsibility (Table 3).

