As part of the comprehensive implant treatment planning process, it’s necessary to think about whether the soft tissue could be optimised at each stage and how this might impact the final result, says Boota Singh Ubhi.
Having established the importance of the soft tissue around dental implants, as well as the range of augmentation techniques available to the modern clinician, it’s vital to understand when each one is most suitable.
Ensuring the right procedure is performed at the right time is essential for enhanced clinical results and patient outcomes.
As part of the comprehensive implant treatment planning process, it’s necessary to think about whether the soft tissue could be optimised at each stage and how this might impact the final result.
Procedures can be performed prior to implant placement, during surgery, after loading or even post restoration. As in every area of dentistry, the most effective timeline for soft tissue intervention will depend on the specific case. It should be assessed on an individual basis.
Effective evaluation will require clinical skill and experience from the practitioner. They will need to either be confident in their own periodontal management capabilities or work with a periodontal specialist for support.
Ultimately, there are three key stages of treatment at which soft tissue augmentation may be performed. Before implant placement, simultaneous with implant placement and post placement.
Before implant placement
Prior to implant surgery, where a lack of gingival volume or keratinised tissue is identified, a connective tissue or free gingival graft may be indicated. The aim of treatment would be to thicken the gingiva and increase volume to a level that would enable full coverage of the implant once placed. This would also help to combat potential recession post implant placement.
Building thicker keratinised tissue around the proposed implant site can also facilitate plaque removal and oral hygiene maintenance post-surgery.
Management of extraction sockets has been a significant area of research in recent years. Preserving and augmenting the connective tissue at time of extraction will create the best environment for implant placement. It will improve osseous properties of the site while encouraging better aesthetics and healing (Deeb and Deeb, 2015).
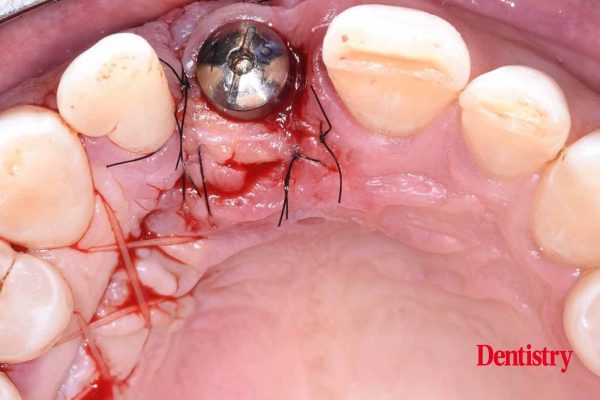
During the surgical procedure
When utilising an immediate implant placement approach or when the tooth is already missing, soft tissue interventions may be performed at time of surgery. The literature suggests that subepithelial connective tissue grafts in these situations can improve aesthetics. They can successfully thicken the peri-implant tissues (Esposito et al, 2012). Indeed, in anterior cases where mid-facial recession is expected, a connective tissue graft may encourage soft tissue stability (Seyssens, De Lat and Cosyn, 2020).
One study found that connective tissue grafts performed simultaneously with implant placement led to 1.3mm thicker soft tissue. Also, significantly improved aesthetics compared to the non-grafted control group (Wiesner et al, 2010). Another study supported findings of significantly improved gingival thickness where a connective tissue graft was performed alongside immediate implant placement and restoration (Atieh and Alsabeeha, 2019).
A pedicle grafting technique is another option for use during the surgical treatment procedure upon exposure of the implant. Research has found a modified approach to provide a safe and predictable soft tissue augmentation solution around maxillary implants, increasing width of keratinised mucosa around the implant site (Salehi et al, 2018).
Post restoration
In some cases, periodontal rejuvenation may be required post-implant placement and restoration. At this point, there are a variety of plastic periodontal techniques that may be applied. The most common are likely once again connective tissue grafts or free gingival grafts.
Where the goal is aesthetic improvement, there is evidence to demonstrate sufficient outcomes with soft tissue grafting (Kassab, 2010). Success has also been shown when performing this grafting after immediate implant placement (in addition to performing simultaneously as already mentioned) (Hsu, Shieh and Wang, 2012). This is true of enhanced aesthetics and soft tissue stability for better healing and long-term outcomes.
The emerging role of biomaterials
There is an array of products and materials on the market to further support surgical treatment and optimise outcomes.
With the majority of soft tissue grafting techniques, the autograft – harvesting tissue from the patient’s donor site – presents the greatest disadvantages in treatment. It creates the need for an extra surgical procedure. This, in turn, significantly impacts healing time, overall treatment time and patient comfort. The advent of biomaterials and grafting substitutes eliminates these issues in a wide selection of cases.
With regards to soft tissue augmentation, the modern practitioner’s arsenal now consists of allografts and xenografts. As you’ll likely know, these are grafts procured from human donors and animal donors. Both remove the need to harvest tissue from the patient for fewer surgeries and greater comfort.
There is also the option to utilise completely synthetic soft tissue grafting materials. These also lessen associated morbidities and reduce surgical time (Toledano et al, 2020).
Developing clinical confidence
While referral to or collaboration with a periodontal specialist may be required in advanced cases, clinicians can undertake training to enable them to improve their soft tissue management with regards to implantology.
The ‘Soft tissue around dental implants’ course with BPI Dental Education and Training is a prime example of a programme that will offer theoretical and hands-on teaching in the field.
It covers all the soft tissue augmentation techniques discussed in this article series and more. It gives clinicians the knowledge and mentorship needed to safely and effectively apply new skills to practice.
At the end of the day, effective soft tissue management is critical for optimal implant outcomes. Being aware of the different augmentation procedures available is important to support the clinical decision-making process. It ensures that every patient gets the very best care.
For references, email guy.hiscott@fmc.co.uk.
This article first appeared on Dentistry magazine. You can read the latest issue here.