Temporomandibular joint and muscle disorder-type pain in U.S. adults: the National Health Interview Survey.
J Orofac Pain. 2008; 22: 317-322
Prevalence, impact, and costs of treatment for temporomandibular disorders. Paper commissioned by the Committee on Temporomandibular Disorders (TMD): from research discoveries to clinical treatment.
in: Yost O. Liverman C.T. English R. Mackey S. Bond E.C. Temporomandibular Disorders: Priorities for Research and Care. The National Academies Press,
Washington, DC2020: C1-C28
Temporomandibular pain and jaw dysfunction at different ages covering the lifespan: a population based study.
Eur J Pain. 2016; 20: 532-540
Longitudinal outcome of temporomandibular disorders: a 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders.
J Orofac Pain. 2003; 17: 9-20
A 20-year longitudinal study of subjective symptoms of temporomandibular disorders from childhood to adulthood.
Acta Odontol Scand. 2001; 59: 40-48
Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients.
Oral Surg Oral Med Oral Pathol. 1985; 60: 615-623
Third molar removal and orofacial pain: a population-based survey.
J Oral Maxillofac Res. 2010; 1: e4
Frequency of dental and traumatic events in the etiology of temporomandibular disorders.
Endod Dent Traumatol. 1988; 4: 182-185
Incident injury is strongly associated with subsequent incident temporomandibular disorder: results from the OPPERA study.
Pain. 2019; 160: 1551-1561
Effect of lengthy root canal therapy sessions on temporomandibular joint and masticatory muscles.
J Dent Res Dent Clin Dent Prospects. 2010; 4: 95-97
Intubation risk factors for temporomandibular joint/facial pain.
Anesth Prog. 2007; 54: 109-114
National Dental PBRN Collaborative Group. Differential diagnoses for persistent pain after root canal treatment: a study in the National Dental Practice-based Research Network.
J Endod. 2015; 41: 457-463
Idiopathic condylar resorption: the current understanding in diagnosis and treatment.
J Indian Prosthodont Soc. 2017; 17: 128-135
Michigan jury awards +850,000 in ortho case: a tempest in a teapot.
Am J Orthod Dentofacial Orthop. 1988; 94: 358-360
Challenges in the clinical implementation of a biopsychosocial model for assessment and management of orofacial pain.
J Oral Rehabil. 2020; 47: 87-100
Multivariable modeling of phenotypic risk factors for first-onset TMD: the OPPERA prospective cohort study.
J Pain. 2013; 14: T102-T115
Assessment of risk factors for oro-facial pain and recent developments in classification: implications for management.
J Oral Rehabil. 2016; 43: 977-989
Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions.
J Pain Res. 2018; 11: 571-587
Assessment of diagnosed temporomandibular disorders and orofacial pain conditions by predoctoral dental students: a pilot study.
J Dent Educ. 2016; 80: 1450-1456
Predoctoral teaching of temporomandibular disorders: a survey of US and Canadian dental schools.
JADA. 2007; 138: 231-237
The National Academies of Sciences Engineering and Medicine. Summary.
in: Yost O. Liverman C.T. English R. Mackey S. Bond E.C. Temporomandibular Disorders: Priorities for Research and Care. The National Academies Press,
Washington, DC2020: 1-15
Principles of risk assessment.
in: Woolf S.H. Jonas S. Kaplan-Liss E. Health Promotion and Disease Prevention in Clinical Practice. 2nd ed. Lippincott Williams & Wilkins,
Philadephia, PA2008: 3-23
Summary of findings from the OPPERA prospective cohort study of incidence of first-onset temporomandibular disorder: implications and future directions.
J Pain. 2013; 14: T116-T124
Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA). Accessed November 30, 2018. https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000761.v1.p1
Study methods, recruitment, sociodemographic findings, and demographic representativeness in the OPPERA study.
J Pain. 2011; 12: T12-T26
Risk factors associated with incidence and persistence of signs and symptoms of temporomandibular disorders.
Acta Odontol Scand. 2010; 68: 289-299
Candidate risk factors for temporomandibular pain and dysfunction syndrome: psychosocial, health behavior, physical illness and injury.
Pain. 1988; 34: 139-151
Comparison of risk factors in patients with acute and chronic orofacial pain.
Anesth Prog. 2018; 65: 162-167
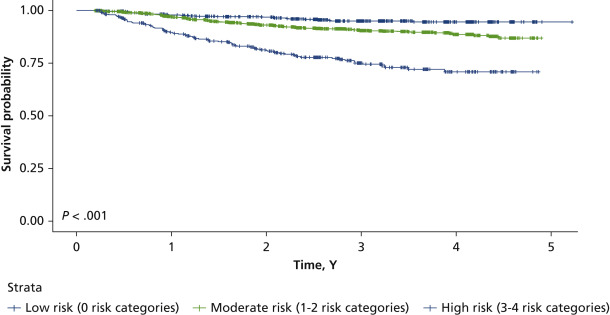
Clinical predictors of persistent temporomandibular disorder in people with first-onset temporomandibular disorder: a prospective case-control study.
JADA. 2019; 150: 572-581.e510
Evaluating the yield of medical tests.
JAMA. 1982; 247: 2543-2546
Validity of three screening questions (3Q/TMD) in relation to the DC/TMD.
J Oral Rehabil. 2016; 43: 729-736
Development of a brief and effective temporomandibular disorder pain screening questionnaire: reliability and validity.
JADA. 2011; 142: 1183-1191
Individual and societal burden of TMDs.
in: Yost O. Liverman C.T. English R. Mackey S. Bond E.C. Temporomandibular Disorders: Priorities for Research and Care. National Academies Press,
Washington, DC2020: 98-139
Risk factors for onset of chronic oro-facial pain: results of the North Cheshire oro-facial pain prospective population study.
Pain. 2010; 149: 354-359
The effect of catastrophizing and depression on chronic pain: a prospective cohort study of temporomandibular muscle and joint pain disorders.
Pain. 2011; 152: 2377-2383
The effect of fibromyalgia and widespread pain on the clinically significant temporomandibular muscle and joint pain disorders: a prospective 18-month cohort study.
J Pain. 2010; 11: 1155-1164
Influence of psychological factors on risk of temporomandibular disorders.
J Dent Res. 2007; 86: 1120-1125
Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort.
J Dent Res. 2013; 92: 70S-77S
Widespread pain as a risk factor for dysfunctional temporomandibular disorder pain.
Pain. 2003; 102: 257-263
Development of temporomandibular disorders is associated with greater bodily pain experience.
Clin J Pain. 2010; 26: 116-120
Preventing chronic pain after acute jaw sprain or strain.
JADA. 2016; 147: 979-986
Psychosocial education improves low back pain beliefs: results from a cluster randomized clinical trial (NCT00373009) in a primary prevention setting.
Eur Spine J. 2009; 18: 1050-1058
Exercise for the primary, secondary and tertiary prevention of low back pain in the workplace: a systematic review.
J Occup Rehabil. 2009; 19: 8-24
Secondary prevention of chronic musculoskeletal pain: a systematic review of clinical trials.
Ann Phys Rehabil Med. 2018; 61: 323-338