Glass polyalkenoate systems (glass-ionomer cements) have remarkable characteristics that make them valuable restorative-dental-repair materials. They are hydrophilic, biocompatible, tooth-colored, and fluoride ion-containing and -releasing. In addition, they form chemical chelation bonds to tooth structure, have a coefficient of thermal expansion similar to tooth structure, and are easily syringe-injected for precision placement in a prepared tooth. The resin-modified type of glass ionomers have enhanced physical characteristics, which make them suitable for use in cases where higher wear resistance and fracture strengths are needed. Changes in glass particle size and distribution also have an influence on the usefulness of the various glass ionomers. An example is the “nano-ionomer.”1
Over time, all glass-ionomer restorative cements are subject not only to wear but also to erosion from acid influences in the mouth. That does not necessarily result in the need to completely replace glass-ionomer restorations that have somewhat deteriorated. Frequently, glass-ionomer restorations can be resurfaced using a bonded, resin-based composite overlay.2 One can consider this treatment “long-term stratification” repair.3 The restoration can be cut down, mechanical undercut retention included, and the original material retained as a dentin-replacement base. This brief pictorial report demonstrates the resurfacing repair of an 8-year-old occluso-buccal restoration in a mandibular permanent molar. Results of the resin-based composite resurfacing are shown at 47 months.
PICTORIAL CASE REPORT
In September of 2008, an 8.5-year-old female had an occluso-buccal repair of her mandibular right permanent first molar. Eight years and 2 months later (December 2016), she was treated for an occlusal caries lesion of the adjacent second molar. Both teeth are pictured preoperatively in Figure 1. After inferior alveolar block anesthesia was achieved and restoration of the second molar completed, the rubber dam retainer was moved to the first molar, and that tooth was isolated. The first molar was then repaired as follows (Figures 2 to 14).
Figure 1. After occlusal repair of the second molar, attention was paid to this 8-year, 2-month-old resin-modified glass ionomer (RMGI) restoration.

Figure 2. The rubber dam was repositioned on the first molar. Wear and erosion is shown on the 8-year-old glass-ionomer restoration.
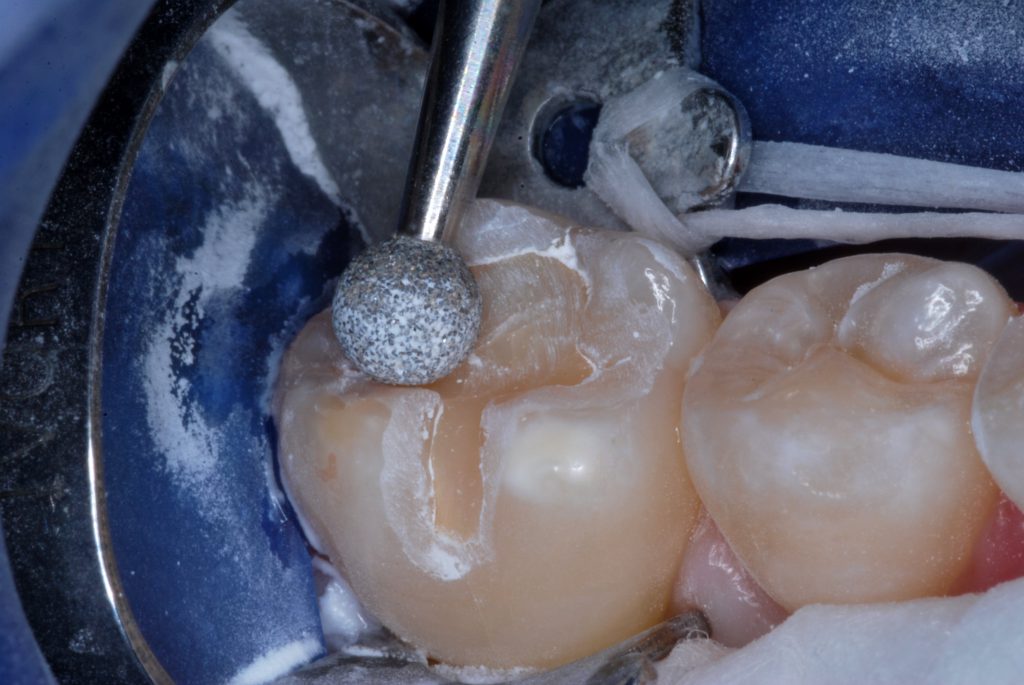
Figure 3. Enamel peripheral to the cavosurface margins was roughened with a large round diamond bur.

Figure 4. A coarse grit cylindrical diamond bur was used to cut the original restoration down 1 to 2 mm and expose the walls of the new preparation. Note the mechanical undercutting of the cavity walls.

Figure 5. The finished preparation for resurfacing. Residual RMGI serves as dentin replacement liner/base.
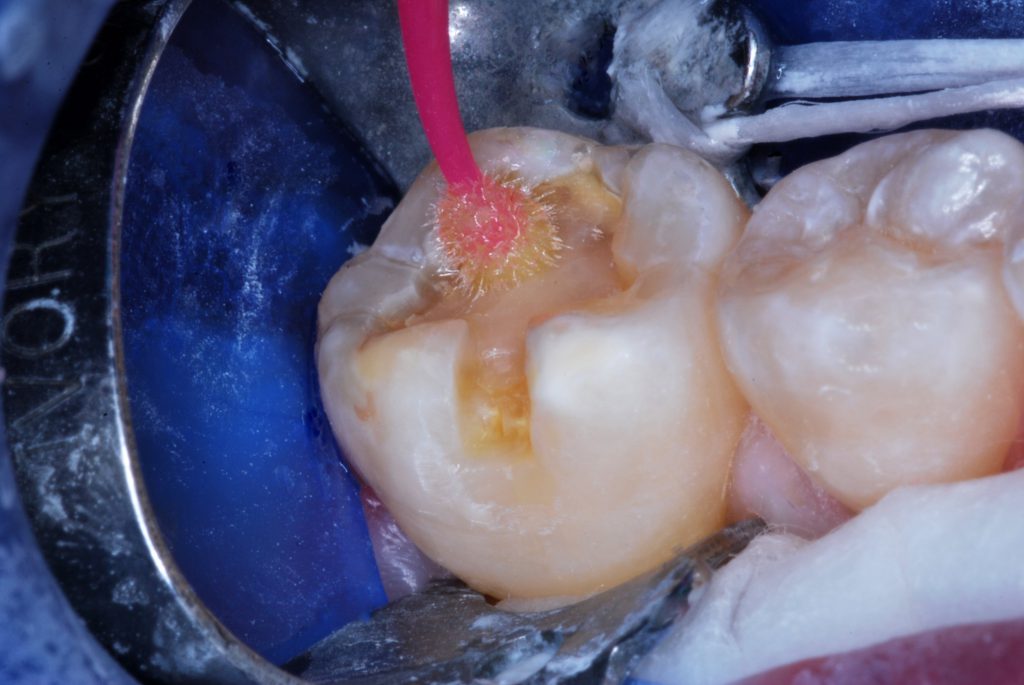
Figure 6. A self-etching bonding agent was applied and agitated for 30 seconds, followed by light beam exposure for 10 seconds (traditional etch/rinse/dry/bond is another option).

Figure 7. Enamel-replacement, resin-based composite was injected with care so as not to incorporate air voids.

Figure 8. Light exposure (1,100 mW/cm2) was done for 20 seconds each from both the buccal and occlusal aspects.

Figure 9. A large round diamond bur at slow speed shaped the occlusal surface.

Figure 10. A resin bonding agent glaze was painted over the restorative surface and peripheral enamel.

Figure 11. Immediately after the final 20-second light beam exposure.

Figure 12. The opposing pointed cusp was smoothed to avoid concentrated impact forces.

Figure 13. Occlusion was evaluated, and needed adjustments were completed.

Figure 14. The resurfaced restoration of the first molar, 47 months postoperatively and 12 years, 2 months after the original tooth repair.
Author’s note: The brand names of materials used in this technique demonstration were not included in this report. The method works well for virtually any type of glass-ionomer system used for dentin replacement that is combined with a suitable adhesively bonded resin-based composite overlay. We consider the mechanical undercutting important to act as an additional retentive form, which assists in fortifying the material against occlusal and masticatory impact forces.
References
1. Killian CM, Croll TP. Nano-ionomer tooth repair in pediatric dentistry. Pediatr Dent. 2010;32(7):530-535.
2. Croll TP, Cavanaugh RR. Resurfacing resin-modified glass-ionomer restorations. Inside Dentistry. 2009;5(1):82-83.
3. Croll TP, Cavanaugh RR. Posterior resin-based composite restorations: a second opinion. J Esthet and Restor Dent. 2002;14:(5)303-312. doi:10.1111/j.1708-8240.2002.tb00526.x
ABOUT THE AUTHORS
Dr. Killian is in private practice of pediatric dentistry in Doylestown, Pa. She earned her DMD degree from the University of Pennsylvania and her Specialty Certificate in Pediatric Dentistry from St. Christopher’s Hospital for Children in Philadelphia. Dr. Killian is an adjunct associate professor of pediatric dentistry at the University of Pennsylvania and a clinical affiliate at The Children’s Hospital of Philadelphia. She is a Fellow and former trustee of the American Academy of Pediatric Dentistry as well as a Diplomate and past president of the American Board of Pediatric Dentistry. She can be reached at cmkillian@aol.com.
Dr. Croll is a Diplomate of the American Board of Pediatric Dentistry. He is a Temple University School of Dentistry graduate, and after 3 years in the US Army Dental Corps, he completed pediatric dentistry training at the University of Connecticut in 1978. Dr. Croll has been in private specialty practice of pediatric dentistry in Doylestown, Pa, since 1978 and became clinical director of Cavity Busters Doylestown, LLC, in December 2018. He is currently an adjunctive clinical professor of pediatric dentistry at the University of Texas Health Science Center in San Antonio and a clinical professor of pediatric dentistry at the Case Western School of Dental Medicine. He can be reached at willipus@comcast.net.
Disclosure: The authors report no disclosures.


