INTRODUCTION
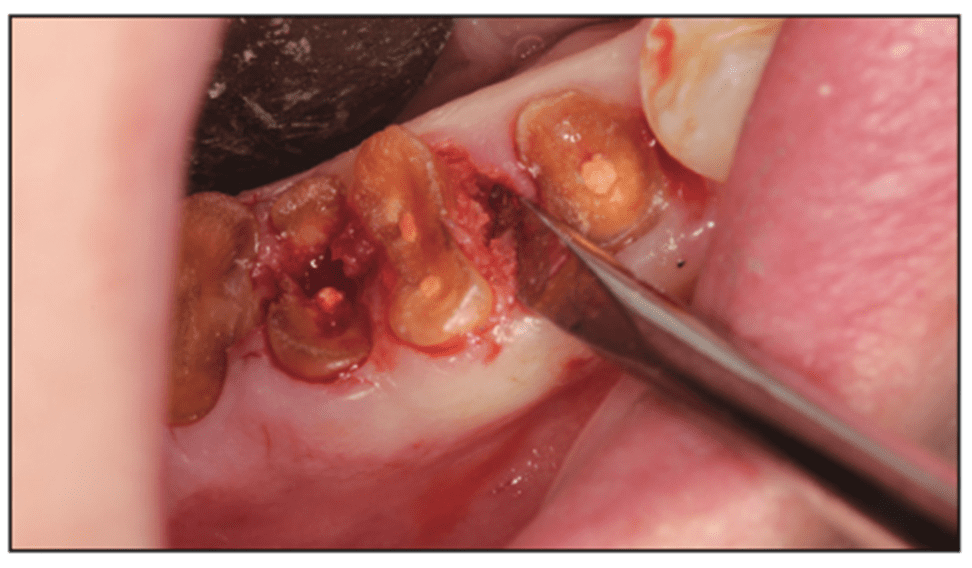
It has been reported that the surgical extraction of a tooth is the most common surgical procedure in the United States.1 A 2015 study by Gilbert et al2 found that 64% of general dentists routinely remove teeth. A common occurrence during tooth removal is a fractured and retained root (Figure 1). At least 11 studies from 1927 to 2007 examined patients with retained roots. Their studies yielded percentages of retained roots from 15% to 37%. An incidental finding was that maxillary molars and premolars fracture the most. Maxillary left molars have the highest proportion of root fractures and oral-antral complications.3
Figure 1. Broken root tip.
This article will address 2 common clinical complications and their recommended solutions. The author would like to note that a plethora of complications could be simply avoided with rigorous patient vetting. Although this article is about clinical complications, recommendations would start by limiting your surgical removal to patients with a medical history that would fall under ASA I and II classification. Maxillofacial surgery offices are better equipped to manage the range of serious medical complications that arise from treating brittle patients. Further, every surgical case performed would be better managed with some level of oral sedation. Anxious patients are more inclined to experience hypertensive episodes. The moment your patient becomes unpredictable in your chair, your clinical skills will be compromised.
BROKEN ROOT TIPS
Keep in mind this important axiom: The primary cause of root tip breakage is too much force in the coronal portion of the tooth, as opposed to the apical region. The best way to prevent root tip breakage is to execute protocols to drive forces apically. This begins with decoronating the crown. The very act of separating the crown from the root trunk creates better vision and access of the roots. Next, it is advised to section the roots. On maxillary molars, this would be the MB from the DB and then the palatal root. On mandibular molars, it would be the MB root from the DB root and then the MB from the ML. Finally, create mesial and distal troughs (not buccal or palatal) and then elevate the roots with any number of the myriad of root tip elevators available. The author defines a trough as a small slot between the root and alveolus that parallels the root.4 The use of dental elevators to remove roots is historically an old concept. When used properly, it allows biomechanical creep to occur, ultimately resulting in bone expansion.5
Modernization of the elevator and root tip picks (another form of an elevator) has dramatically improved the ability of today’s clinicians to both avoid root breakage and elevate remaining root tips, if broken. Salvin Dental Specialties and Hu-Friedy both have wide arrays of elevators to execute these principles (Figure 2). It is recommended that a Brasseler 859.36.010 bur (Brasseler USA) on a high-speed drill be employed to create the trough (Figure 3). Even then, all surgeons experience root tip breakage.
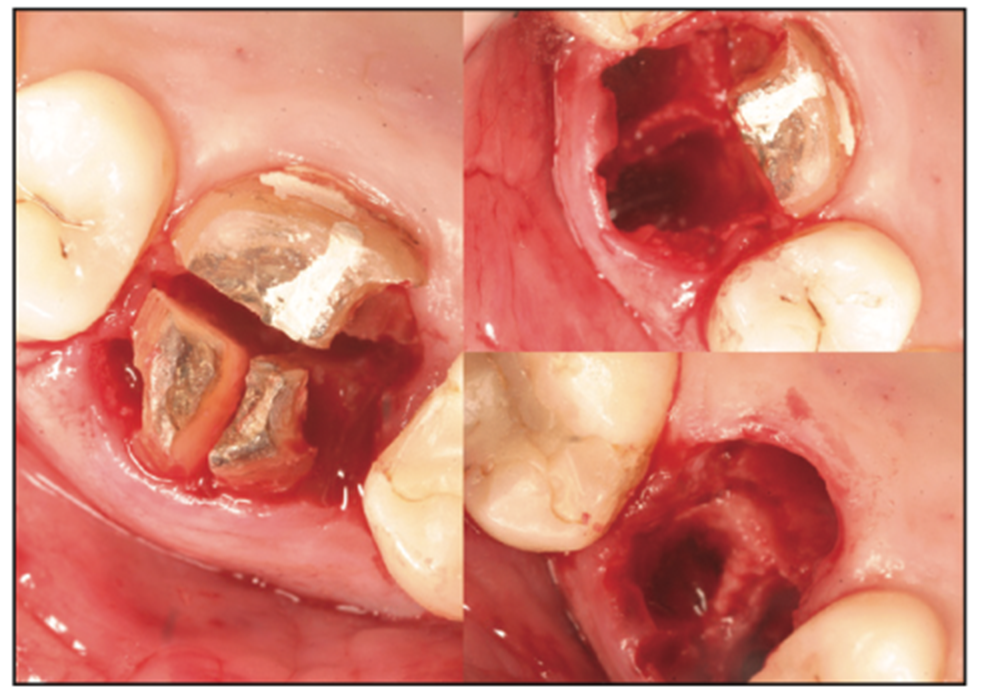
Figure 2. Sectioning for prevention.
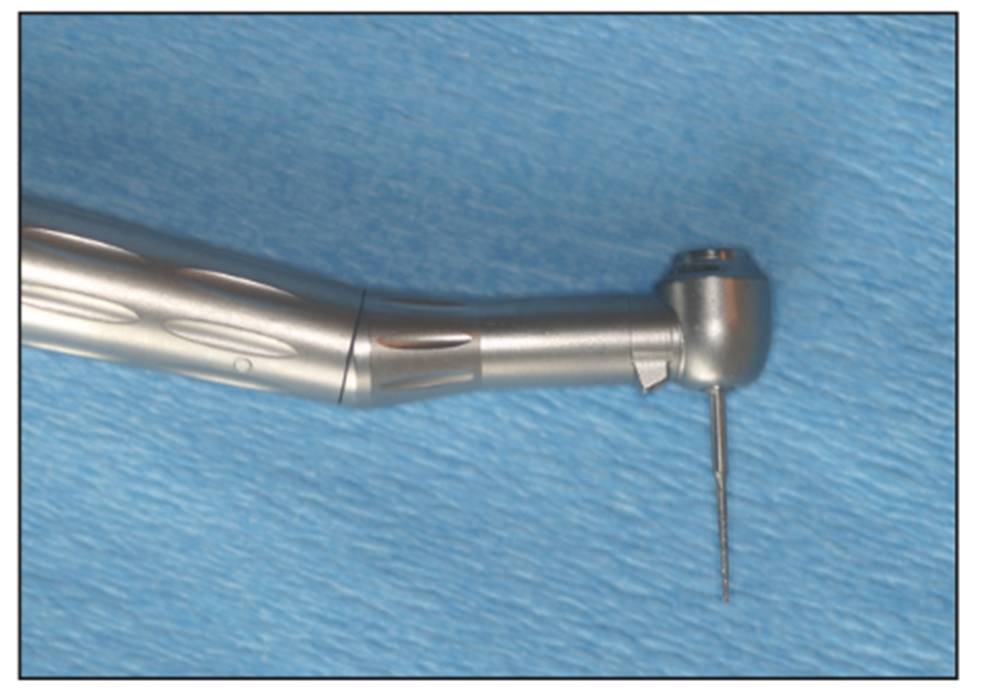
Figure 3. The Brasseler 859.36.010 bur (Brasseler USA).
Recommended Solution
Vision and Access: Creating a small flap one tooth mesial and distal to the tooth to be removed will instantly improve the ability of the clinician to see and access the area. Retrieving a broken root tip requires magnification and surgical enhanced lighting to eliminate shadows in the working field.
Once the surgical site can be clearly inspected, a trough (1.0 mm) mesial and/or distal around the broken root tip is created. The trough in the bone parallels the root to at least half of its length. This space allows the use of root tip elevators to then torque the root until it is easily retrieved (Figure 4). The root tip elevator is essential for the broken root tip. It is important once the root is engaged that a constant—not back and forth—torque with the elevator is applied for 10 seconds (Figures 5 and 6).
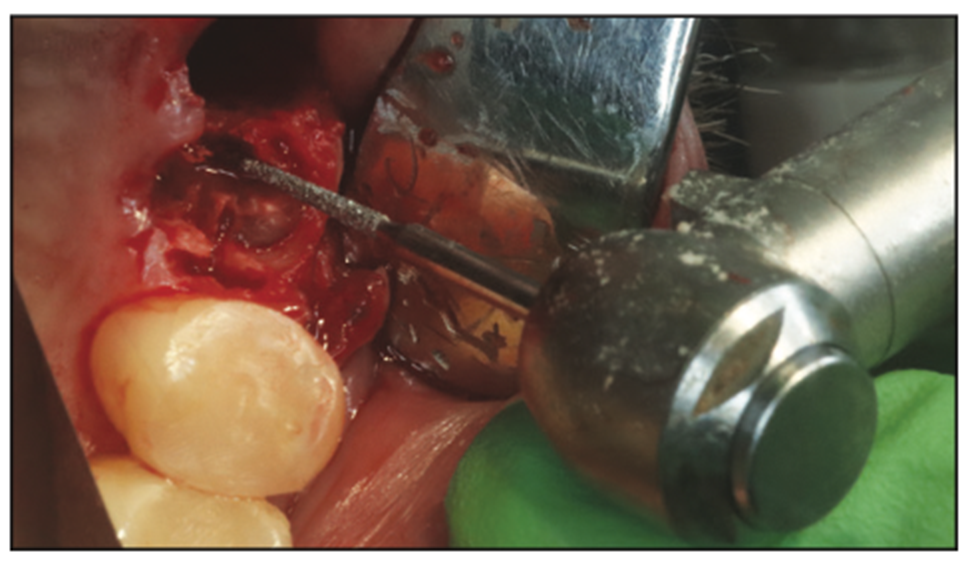
Figure 4. Creating the trough.

Figure 5. Examples of the wide range of available root tip elevators.

Figure 6. Elevator inserted in trough. Torque 10 seconds for elevation.
Leaving the root tip: Historically, there was a consensus that “all root tips should be removed. Not doing so would lead to pain, infection, and cyst development.”3
In the past 11 years, there has been abundant literature weighing in on the outcome of leaving retained roots. It is a concept reviewed as early as 1960 by Helsham,6 who examined 2,000 patients referred for the removal of retained roots. He found that most retained roots “develop tissues that heal over them and there was a progression of root canal closure and fibrosis of the pulp.”6
He further concluded that 83% were associated with neither symptoms nor pathology. It is worth noting that sometimes vital roots are intentionally retained for improved prosthetic outcomes. Roots are reduced 2.0 mm subosseously to preserve bone. These roots undergo typical wound closure and healing.3
Conversely, there is clear evidence that if the broken root tip is left in, communication with the oral cavity as opposed to sequestered in the bone, the incidence of complications increases. These complications include local inflammation, cyst formation, and pain.7
Risk Assessment
One governing aspect in the clinician’s decision tree is the consideration of further danger to surrounding anatomy that would adversely impact the outcome by removing the root fragment. Perforation of the maxillary sinus, injury to the inferior alveolar bundle, and injury to the mental foramen are 3 common examples. This is precisely the theory behind the coronectomy approach of third molars: to avoid the IAN bundle.8,9
Conclusion and Guidelines
1. Literature review does not identify the size of the remaining fragment as a factor in the final decision to leave a root fragment.
2. Non-vital fragments with periapical pathology communicating with the oral cavity should be removed.
3. Healing of the fractured root is favorably influenced by vitality of the root and its non-mobility from the extraction process.3
MAXILLARY SINUS PERFORATION
Some studies have suggested that 50% of maxillary molars maintain roots that line the wall separating the oral-antral cavities.10 During the removal of these teeth, an oral-antral communication (OAC) can occur. A 2019 article by Parvini et al11 revealed the following: Maxillary second molar extractions result in 5% of OACs; third molars, 30%; first molars, 27.2%; and first premolars cause 5.3%. Additionally, a 2001 study by Hirata et al12 reviewed 2,038 teeth removed from 1,337 patients. This study observed a rate higher in males with 5.2% over females at 3%. Sinus perforations increased gradually with age and occurred most often in the third decade of life.. Sinus perforation was highest with the removal of the first maxillary molar.12 It is anecdotal from my experience with numerous live clinics that many clinicians are surprised when they do encounter a torn sinus following the extraction and are often unsure of the proper clinical approach.
What If You Are Uncertain or Unaware of a Breach?
Visual inspection is one way to identify an OAC. As stated, this requires high magnification and headlamps. However, most experienced clinicians have encountered in real-time, or postsurgical times, situations where it wasn’t clear if the sinus was breached. The escape of fluids and air from the mouth into the nose, unilateral congestion, or a yellow discharge are common patient reports if a sinus has been violated. The first clinical response should be to not poke or explore the suspected tear. A literature review also reveals the “nose blowing test” as a common exercise to confirm an opening. The patient is asked to blow through his or her nose as he or she pinches his or her nostrils together. The presence of blood or mucoid secretions in the mouth as they travel through the opening is evidence of a tear.13
Solutions to OAC
Treatment of the OAC is dependent on the size of the perforation (Figure 7).
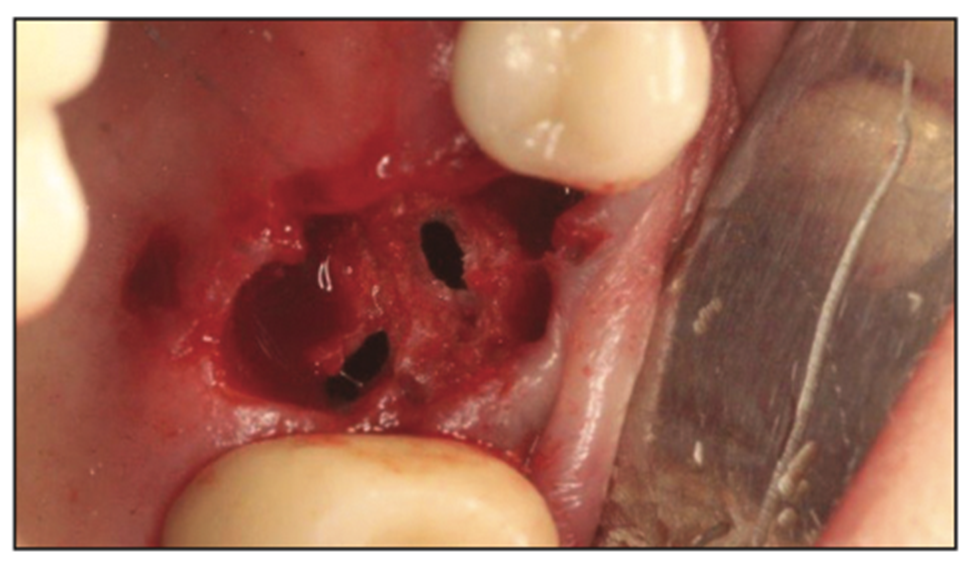
Figure 7. Sinus perforations in the 2.0- to 5.0-mm range.
1. At 2.0 mm or less: If there is no known sinus infection, these defects can resolve on their own following blood clot formation and secondary healing.14 However, larger tears will lead to acute maxillary sinusitis within 48 hours in 50% of the patient population. Some clinicians treat the smaller tears by placing a collaplug in the socket and prescribing an antibiotic regimen of Augmentin 850 mg (20 tablets) twice daily until all used, along with Sudafed ER decongestant.14 If allergic, the following alternate Rx is recommended: Levofloxacin 400 mg BID per OS until 72 hours to symptoms remission. This prescription will be part of all 3 approaches covered in the article.
2. From 2.0 mm to 5.0 mm: Cover the floor of the socket over the tear with a long-lasting (cross-linked) collagen membrane. Cross-linked collagen typically absorbs in 36 weeks. Mem-Lok (BioHorizons) is an easy-to-handle membrane that has provided consistent outcomes. The second layer would again be collagen in the form of a plug. The collagen should then be stitched with an “X” type of suture with a non-resorbable PTFE-type suture. This suture is far less likely to attract any type of bacterial wick.
3. Greater than 5.0 mm: Follow the protocol described above, but add a third layer of dense PTFE membrane tucked in the buccal and palatal flaps 4 to 5 mm past the buccal and palatal crests of bone. This membrane can safely be exposed to the oral cavity. Leave in place for 4 to 6 weeks. This will provide the same outcome as primary closure from the patient’s own tissue. The advantage of this approach will be that it does not require primary closure and will not alter the depth of the natural vestibule. Although there are many dense PTFEs commercially available, Osteogenics has a wide array of both PTFE membranes and sutures (Figure 8).
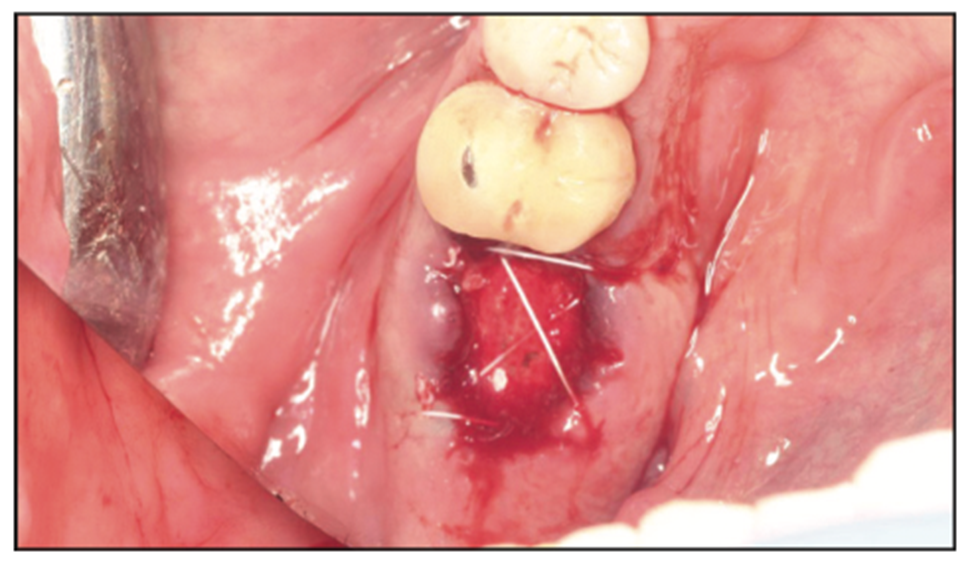
Figure 8. Oral-antral communication closed with dense PTFE.
CONCLUSION
Root tip fractures and OACs are not uncommon complications. As with all complications, prevention is the best solution. Part of a clinician’s protocol prior to removal should be a strategy and risk assessment of the tooth to be removed: Does the tooth have a history of a root canal? Is the tooth in dense bone? Perhaps, this is a patient with parafunction and buccal buttresses of bone? Are the roots longer than average? Do the roots line the maxillary sinus? In the rigorous routine of daily practice, it wouldn’t be unusual for the clinician to proceed with an extraction without this beneficial review. Exercising a strategy session allows for preparation—including the proper, and potentially needed, armamentarium—or even a referral. If the clinician removes enough teeth, they will encounter one or both of these complications. It is the responsibility of the clinician to manage the complication within the standard of care.
REFERENCES
1. Colgate. When surgical extraction of teeth is necessary.
2. Gilbert GH, Gordan VV, Korelitz JJ, et al; National Dental PBRN Collaborative Group. Provision of specific dental procedures by general dentists in the National Dental Practice-Based Research Network: questionnaire findings. Tex Dent J. 2016;133(12):726–46.
3. Nayyar J, Clarke M, O’Sullivan M, et al. Fractured root tips during dental extractions and retained root fragments. A clinical dilemma? Br Dent J. 2015;218(5):285–90. doi:10.1038/sj.bdj.2015.147
4. Rasner SL. A modern approach to exodontia, part 1: Helping to ensure successful implant outcomes. Dent Today. 2018;37(1)108-113.
5. Misch CE, Suzuki JB. Tooth extraction, socket grafting, and barrier membrane bone regeneration. Contemporary Implant Dentistry, 3rd ed. St. Louis, MO: Mosby; 2007:870-874.
6. Helsham RW. Some observations of the subject if roots of teeth retained in the jaws as a result of incomplete. Aust Dent J. 1960;5:70–7. doi: 10.1111/j.1834-7819.1960.tb03154.x
7. Glickman I, Pruzansky S, Ostrach M. The healing of extraction wounds in the presence of retained root remnants and bone fragments: an experimental study. Am J Orthodontics Oral Surg. 1947;33:263–83. doi:10.1016/0096-6347(47)90063-x
8. Patel V, Moore S, Sproat C. Coronectomy — oral surgery’s answer to modern day conservative dentistry. Br Dent J. 2010;209(3):111–4. doi:10.1038/sj.bdj.2010.673
9. Renton T, Hankins M, Sproate C, et al. A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg. 2005;43(1):7-12. doi:10.1016/j.bjoms.2004.09.002
10. Howe, GL. Some complications of tooth extraction. Ann R Coll Surg Engl. 1962;30(5):309–23.
11. Parvini P, Obreja K, Begic A, et al. Decision-making in closure of oroantral communication and fistula. Int J Implant Dent. 2019;5(1):13. doi:10.1186/s40729-019-0165-7
12. Hirata Y, Kino K, Nagaoka S, et al. [A clinical investigation of oro-maxillary sinus-perforation due to tooth extraction]. Kokubyo Gakkai Zasshi. 2001;68(3):249-53. Japanese. doi:10.5357/koubyou.68.249
13. Haanaes HR, Pedersen KN. Treatment of oroantral communication. Int J Oral Surg. 1974;3(3):124-32. doi:10.1016/s0300-9785(74)80043-8
14. Khandelwal P, Hajira N. Management of oro-antral communication and fistula: various surgical options. World J Plast Surg. 2017;6(1):3-8.
ABOUT THE AUTHOR
Dr. Rasner earned his DMD degree from the University of Pennsylvania. He has completed the Misch International Implant Institute curriculum and the Pikos Institute continuum. Dr. Rasner has been teaching for 20 years. His courses, “Atraumatic Extractions for the GP” and “The Bulletproof Guide to Implant Success,” have been popular at ADA and AGD component society meetings, as well as at the national ADA meeting. His newest course, “Hands-on Atraumatic Extractions for the GP,” features 2 days of live-patient experience in his office. He has authored 3 books and more than 50 industry and journal publications. He can be reached at drrasner@aol.com.
Disclosure: Dr. Rasner reports no disclosures.