Esthetic Dilemma of the Gingival Margin
The data is unambiguous; both porcelain and composite resin are biocompatible with the gingiva and well tolerated.1-3 The caveat is that composite tends to cause tissue irritation if it comes into intimate contact with the gingiva.4-6 This ultimately causes unesthetic gingival recession. Porcelain is less problematic, but plaque build-up at the margin, reacting to the thin layer of resin cement, leads to a similar free gingival irritation and, eventually, recession.7,8
Even careful subgingival margin placement will all too often, within a short span of 3–5 years, due to aging, gingival irritation, or lack of home maintenance on the patient’s part, lead to unesthetic recession and full visible exposure of the darker dentinal tissue.9,10 Thus, the restorative conclusion is to locate composite resins supragingivally,3,11 with the composite reasonably away (0.25-0.50mm) from periodontal structures and thereby unlikely to cause tissue irritation.
With currently available adhesives and restoratives, this is a rather straightforward task.12-19 Later generation adhesives bond equally well, and predictably, to both enamel and dentin.14,15 Significantly, 7th and 8th generation adhesives have similar bonding strengths to both enamel and dentin, eliminating the potential stresses caused by unequal polymerization contraction.17-19 It is clinically possible to create a continuous lasting restoration through the dentino-enamel junction (DEJ), covering as much of the enamel and the dentin as necessitated by decay or abfraction (or both).
The esthetic predicament quickly becomes evident, however. Dental restorative materials are designed to match the shade of the enamel portion of the tooth. While some manufacturers offer “dentin” shades, these hues typically do not closely match the darker coloration of exposed dentin, particularly in endodontically treated teeth. A substantial increase in the apparent length of a tooth, specifically in the anterior labial region, detracts from the esthetic smile. A typical central incisor measures approximately 10.5mm cervico-incisally (CI).20
To restore a Class V decay or abfraction, or perhaps a small gingival recession, an enamel-colored resin is placed at the labial DEJ. Increasing the maxillary central incisor’s vertical aspect (Fig. 1) by a mere 3mm adds 30% to the apparent vertical dimension, significantly altering the cervico-incisal to mesio-distal (CI:MD) ratio, totally upsetting the esthetic parameters of the smile. (Fig. 2) In situations where there is even moderate (not even considering extensive) recession, the visual imbalance is even further impaired. The CI:MD ratio impact is even greater on maxillary laterals and mandibular incisors (average 9.0mm CI). Maxillary and mandibular cuspids (average 10-11mm CI) are often the teeth most affected by gingival recession, and are also highly visible both anteriorly and laterally.
Fig. 1
Normal length maxillary central incisors – expected appearance.
Fig. 2

Maxillary incisors apparent length increased by 30% – very unnatural and unesthetic.
Individuals who have gingival recession, abfraction and/or decay tend to look older than they really are (long in the tooth). Covering the darker root dentin with an enamel-shaded resin simply makes their teeth more visible, seemingly longer, and correspondingly less esthetic.
The practitioner’s dilemma is how to solve this problem practically, esthetically, and with minimum invasiveness. The restoration must be functional, replacing missing dental structures to natural dimensions and contours. The restoration should restore lost enamel with enamel-shaded composite resin, and receded gingiva with gingival-shaded composite resin. By creating an artificial enamel-gingival junction in composite restorative material, the patient’s esthetics and smile can be restored.
Solving the Gingival Esthetic Dilemma
Beautifil II Gingiva (Shofu USA, San Marcos CA) has been specifically designed for the re-balancing of pink aesthetics in the cervical areas of the dentition. (Fig. 3) Beautifil II Gingiva is indicated for wedge-shaped defects, cervical decay, the esthetic rectification of gingival recession, shielding exposed cervical areas and splinting of mobile teeth. The resin material is available in 5 tones (dark pink, light pink, brown, orange and violet) (Fig. 4) which can be layered and/or blended to achieve custom shades that allow the treatment of patients with various hues of gingival pigmentation, according to their clinical needs. (Fig. 5)
Fig. 3

Beautifil II Gingiva Shades (Shofu USA, San Marcos CA).
Fig. 4

The resin material is available in 5 shades (dark pink, light pink, brown, orange and violet).
Fig. 5

Resins layered and/or blended to achieve custom gingival shades.
Beautifil II is a highly esthetic, fluoride-releasing composite resin material indicated for all classes of restorations. Numerous studies over the past 20 years have shown no secondary caries, no failures, no post-operative sensitivity and a high retention of both color match and surface luster. The material is based on Shofu’s proprietary Giomer technology. (Fig. 6) The significant advantage of the Giomer class of resins is that they not only release fluoride to protect the tooth at the restorative margin, but that their fluoride content can be recharged by toothpastes, fluoride rinses and varnishes. Thus, the Giomer’s fluoride releasing capacity does not decrease over time.
Fig. 6

Giomers continue to release fluoride because their fluoride content can be recharged with fluoride toothpastes, rinses and varnishes.
Another important consideration is that the gingival margin of the restorative material (whether pink or enamel in color) must be kept supragingival and slightly away from the free gingival margin.3,4,6 While a very narrow band of darker root structure may be visible towards the apex, the restoration’s enamel (coronal) and pink gingival (radicular) coloration will focus attention away from this area. With gingivally blended restorations, the professional can deliver both esthetic and supragingival margins within the same restoration. A supragingival margin facilitates ready access and effective home maintenance for the patient.
It is imperative that a restoration that is so close to the free gingival margin be placed under conditions controlled for moisture and bleeding. Rubber dam placement is impractical (target area is positioned apically) and retraction cord may physically or chemically compromise the working area. Ideally, the patient’s oral hygiene creates a healthy gingival microenvironment, with minimal pocketing and no bleeding on probing. In most cases, however, the practitioner must modify the actual situation to increase the likelihood of clinical success. The easiest and best technique for predictable tissue sculpting is the use of the diode laser.21,23 Utilizing low power (1.0-1.5 watts), the dentist can produce an ideal, dry, clean, and blood-free working area in less than a minute.
Clinical Cases
Visible Recession and Decay
Remarkably, the patient’s chief concern was the gingival recession on the left maxillary lateral, not the mesial caries. (Fig. 8) Fortunately, the patient’s oral hygiene was relatively good, and restoring the MLB decay was straightforward (BeautiBond (Fig. 7) and Beautifil Flow Plus X, both from Shofu USA, San Marcos CA). The steps for the esthetic rectification of the buccal recession are:
- Gently micro-abrade the receded area and the apical enamel to remove food debris and plaque. The nozzle of the abrader should be angled incisally to prevent gingival irritation and bleeding. Rinse thoroughly and lightly air dry, leaving the surface slightly moist (although the degree of moistness is not critical).
- Apply BeautiBond, a 7th generation dental adhesive, and leave for 10 seconds. Thoroughly air dry the adhesive (very critical). Light cure.
- Select the appropriate Beautifil II Gingiva shade (Light Pink and Violet for this patient) and apply to the receded area to restore the buccal dimension and contour of the original soft tissue. Light cure. It is important to leave a small (0.25-0.50mm) gap between the apical margin of the restorative and the free gingival margin. (Fig. 9) This space prevents gingival irritation, is easily maintainable by the patient, and is generally not visible even with close-up photographs. (All photography
done with the Shofu EyeSpecial camera, (Fig. 10) Shofu USA, San Marcos CA.)
Fig. 7

BeautiBond 7th generation dental adhesive.
Fig. 8
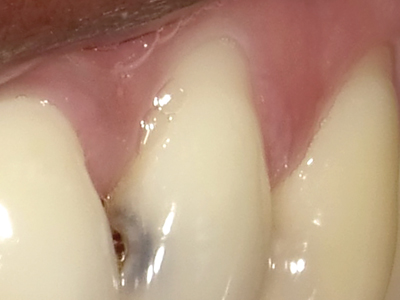
Maxillary left lateral with decay and recession.
Fig. 9

Maxillary left lateral with mesial restoration and gingival restorative rectification.
Fig. 10

EyeSpecial Dental Camera (Shofu USA, San Marcos CA).
Mandibular Anteriors Recession
This is the most commonly encountered recession in the oral cavity. The mandibular anteriors are small, close together, and not effectively cleaned by the tongue and the lower lip. (Fig. 11) Due to gravity, food debris and plaque tend to accumulate labially and interproximally. (Fig. 12) In this case, the major culprit for the recession is the frenum that pulls the attached gingiva apically. The preliminary process is a diode laser frenectomy to eliminate the muscular forces.21-23 The steps for the esthetic rectification of the buccal recession are:
- Gently micro-abrade, in an incisal direction, the receded areas and the enamel nearest to the DEJ to remove food debris and plaque. Rinse thoroughly and lightly air dry, leaving the surface slightly moist.
- Apply BeautiBond and leave for 10 seconds. Thoroughly air dry the adhesive. Light cure.
- Select the appropriate Beautifil II Gingiva shade (Light Pink in this case) and apply to the receded area to restore the buccal dimension and contour of the original soft tissue. Light cure. Leave a small (0.25-0.50mm) gap between the apical margin of the restorative and the free gingival margin. (Fig. 13) This procedure restores the expected gingival height, and contributes to making the patient’s smile look younger.
Fig. 11

Mandibular anteriors with labial gingival recession.
Fig. 12

Mandibular anteriors close-up.
Fig. 13

Mandibular anteriors with gingival restorative rectification.
Conclusion
Beautifil II Gingiva enables the practitioner to overcome the gingival esthetic dilemma. The esthetic gingival restoration technique is predictable and can typically be accomplished without the need for local anesthetic or discomfort to the patient. These restorations are totally functional and replace both hard and soft missing dental structures to natural dimensions and contours with minimum invasiveness. The restoration of the coronal anatomy with tooth-colored composite resins is well established; the development of an artificial enamel-gingival junction and the reconfiguration of missing gingival structures with composite resins is a novel solution that restores the patient’s smile and facial esthetics.
Oral Health welcomes this original article.
References
- Freedman G: Ultraconservative Porcelain Veneers, Esthet Dent Update 2:224-228, 1997.
- Freedman G: Ultraconservative Rehabilitation, Esthet Dent Update 5:80-85, 1991.
- Freedman G, Fugazzotto PA, Greggs TR: Aesthetic Supragingival Margins, Pract Periodontics Aesthet Dent 2:35-38, 1990.
- Newcomb GM: The Relationship Between the Location of Subgingival Crown Margins and Gingival Inflammation, J Periodontol 45:151, 1974.
- Renggli H, Regolati B: Gingival Inflammation and Plaque Accumulation by Well Adapted Supragingival and Subgingival Proximal Restorations, Helv Odont Acta L6:99, 1972.
- Waerhau SJ: Histologic Considerations which Govern where the Margins of Restorations Should be Located in Relation to the Gingiva, Dent Clin North Am 4:161, 1960.
- Berman M: The Complete Coverage Restoration and the Gingival Sulcus, J Prosthet Dent 29:1301, 1973.
- Marcum O: The Effect of Crown Margin Depth upon Gingival Tissues, J Prosthet Dent 17:479, 1967.
- Freedman GA, McLaughlin G: The Color Atlas of Porcelain Laminate Veneers, St Louis, Ishiyaku EuroAmerica, 1990.
- Freedman G: Contemporary Esthetic Dentistry, Elsevier Publishing, 2011 Chap 23; 551.
- Freedman G, Klaiman HF, Serota KT, et al: EndoEsthetics: Part II. Castable Ceramic Post and Core Restorations. Ont Dent 70:21-24, 1993.
- Albers HF: Dentin-resin bonding. Adept Report 1990; 1:33-34.
- Munksgaard EC, Asmussen E. Dentin-polymer Bond promoted by Gluma and various resins. J Dent Res 1985; 64:1409-1411.
- Barkmeier WW, Erickson RL: Shear bond strength of composite to enamel and dentin using Scotchbond multi-purpose. Am J Dent 1994; 7:175-179.
- Swift EJ, Triolo PT: Bond strengths of Scotchbond multi-purpose to moist dentin and enamel. Am J Dent 1992; 5:318-320.
- Gwinnett AJ: Moist versus dry dentin; its effect on shear bond strength. Am J Dent 1992; 5:127129.
- Freedman G, Leinfelder K: Seventh Generation Adhesive Systems. Dentistry 2003; January:15–18.
- Freedman G: 7th generation Adhesive Systems. Dental Asia (English) 2019; March-April:50-53.
- Freedman G: Adhesion: Past, Present, and Future. Oral Health 2019: July 109:7 8-14,82.
- Wheeler RC: A Textbook of Dental Anatomy and Physiology. W.B. Saunders 1965: 6:126.
- Goldstep F: Soft Tissue Diode Laser: Where Have You Been All My Life?. Oral Health 2009: 99:7;34-38.
- Goldstep F: Diode Lasers for Periodontal Treatment: The Story So Far. Oral Health 2009: 99:12;44-46.
- Goldstep F: Diode Lasers: The Soft Tissue Handpiece. Dental Asia 2011: Jan-Feb; 28-32.
About the Author
 Dr. George Freedman is co-founder and past president, American Academy of Cosmetic Dentistry; co-founder, Canadian AED; Regent and Fellow, International Academy for Dental Facial Esthetics, and Diplomate and Chair, American Board of Aesthetic Dentistry. Adjunct Professor, Dental Medicine, Western University, Pomona CA and Professor/Program Director, BPP University, London, UK, MClinDent Programme, Restorative and Cosmetic Dentistry.
Dr. George Freedman is co-founder and past president, American Academy of Cosmetic Dentistry; co-founder, Canadian AED; Regent and Fellow, International Academy for Dental Facial Esthetics, and Diplomate and Chair, American Board of Aesthetic Dentistry. Adjunct Professor, Dental Medicine, Western University, Pomona CA and Professor/Program Director, BPP University, London, UK, MClinDent Programme, Restorative and Cosmetic Dentistry.
 Dr. Paiman Lalla, graduate of University of The West Indies, received his AEGD (Lutheran Medical Center) and Fellowships in the International Congress of Oral Implantology and American Academy of Implant Prosthodontics. He practises in Trinidad & Tobago and serves on the Medical Panel, Ministry of National Security.
Dr. Paiman Lalla, graduate of University of The West Indies, received his AEGD (Lutheran Medical Center) and Fellowships in the International Congress of Oral Implantology and American Academy of Implant Prosthodontics. He practises in Trinidad & Tobago and serves on the Medical Panel, Ministry of National Security.
RELATED ARTICLE: Armamentarium and Techniques For the Immediate Restoration of Endodontically Treated Teeth


