Creating Aesthetics for the Young Cosmetic Dental Patient in the Social Media Era
INTRODUCTION
Younger patients are seeking cosmetic dentistry now more than ever. With the popularity of social media platforms such as TikTok, Instagram, and YouTube, many younger adults want a beautiful and dynamic smile to elevate their facial beauty, drive more attention to their posts, and increase their number of followers and subscribers. During this time of instant gratification, younger patients want cosmetic dental procedures to be done quickly.
Thus, minimally invasive composite resin veneers have become popular during this post-COVID-19 surge.
CASE REPORT
The patient was an 18-year-old female who presented with congenitally misshapen teeth (Figures 1 and 2). This patient did not like her aggressive canine, undersized lateral incisors, and unfeminine smile. The patient wanted a more uniform size and shape of her teeth to create a beautiful facial impact.
To show the patient the possibilities of her new smile, a diagnostic wax-up was hand-sculpted by the clinician and shown to her. A diagnostic wax-up is a great 3D tool to help patients assess the vision of the dentist. Aesthetics are a subjective aspect of dentistry; therefore, it is important that the dentist and the patient have the same vision for the aesthetic results prior to starting the cosmetic dental procedure.
Figure 1. This young female patient presented with congenitally mis-shapened teeth. She didn’t like the aggressive canine, undersized lateral incisors, and unfeminine smile.

Figure 2. The patient’s unaesthetic smile created a teenage appearance that she disliked. She wanted to create a dynamic appearance for social media purposes.
After a discussion with the patient, it was determined that full-contoured composite resin veneers would produce minimal trauma to the tooth, maximum protection due to total sealing with adhesive bonding, and a minimally invasive solution to the existing problem.1,2
In addition, this would be a one-appointment procedure, meeting the patient’s need for speedy resolution. Having a fast, painless, dynamic solution that can be completed in the least number of appointments possible is the best option for the demanding, young cosmetic dental patient.
After accepting the treatment plan, pretreatment preparations were done to prepare for the direct composite resin veneers procedure. The amount of tooth preparation was predetermined on the diagnostic model to attain minimal invasiveness.
To re-create the lingual and incisal contours of the central incisors, a PVS impression was taken only along the lingual and incisal aspects of the diagnostic wax-up. This PVS matrix is also used as a preparation guide, so only a minimal amount of tooth structure was removed to accomplish the goals of the new smile design (Figure 3).

Figure 3. This PVS matrix was also used as a preparation guide, so only minimal tooth structure was removed prior to the veneer procedure.
Isolation of the area was achieved with an OptraGate (Ivoclar Vivadent). A thin retraction cord (4-0 suture cord [Patterson Dental]) was placed along the facial aspect in the gingiva to create a contamination-free environment prior to performing the procedure.
When performing a smile design, it is important to first restore both central incisors, which sets the stage in the new smile design. After the central incisors are completed, the clinician sequentially restores the lateral incisors and canines together. Then, if needed, the premolars are the last teeth to be veneered.
Full-Contoured Composite Resin Veneer Procedure
First, the enamel surface was cleaned with a microetcher (MicroEtcher II [Zest Dental Solutions]) to remove all dental pellicle from the tooth surface. Then, using a selective-etch technique, the enamel was etched with 32% phosphoric acid with benzalkonium chloride (Select HV Etch with BAC [BISCO Dental Products]).
It is important to ensure the adjacent teeth are not etched, so a clear matrix was placed interproximally for protection prior to etching. An all-in-one adhesive resin (G-Premio BOND [GC America]) was used as the adhesive bonding resin. One to 2 layers of G-Premio BOND were placed for 10 seconds, then blown thin using forced air for 5 to 10 seconds. The adhesive was light-cured for 10 to 15 seconds on both the facial and lingual sides (Figure 4).
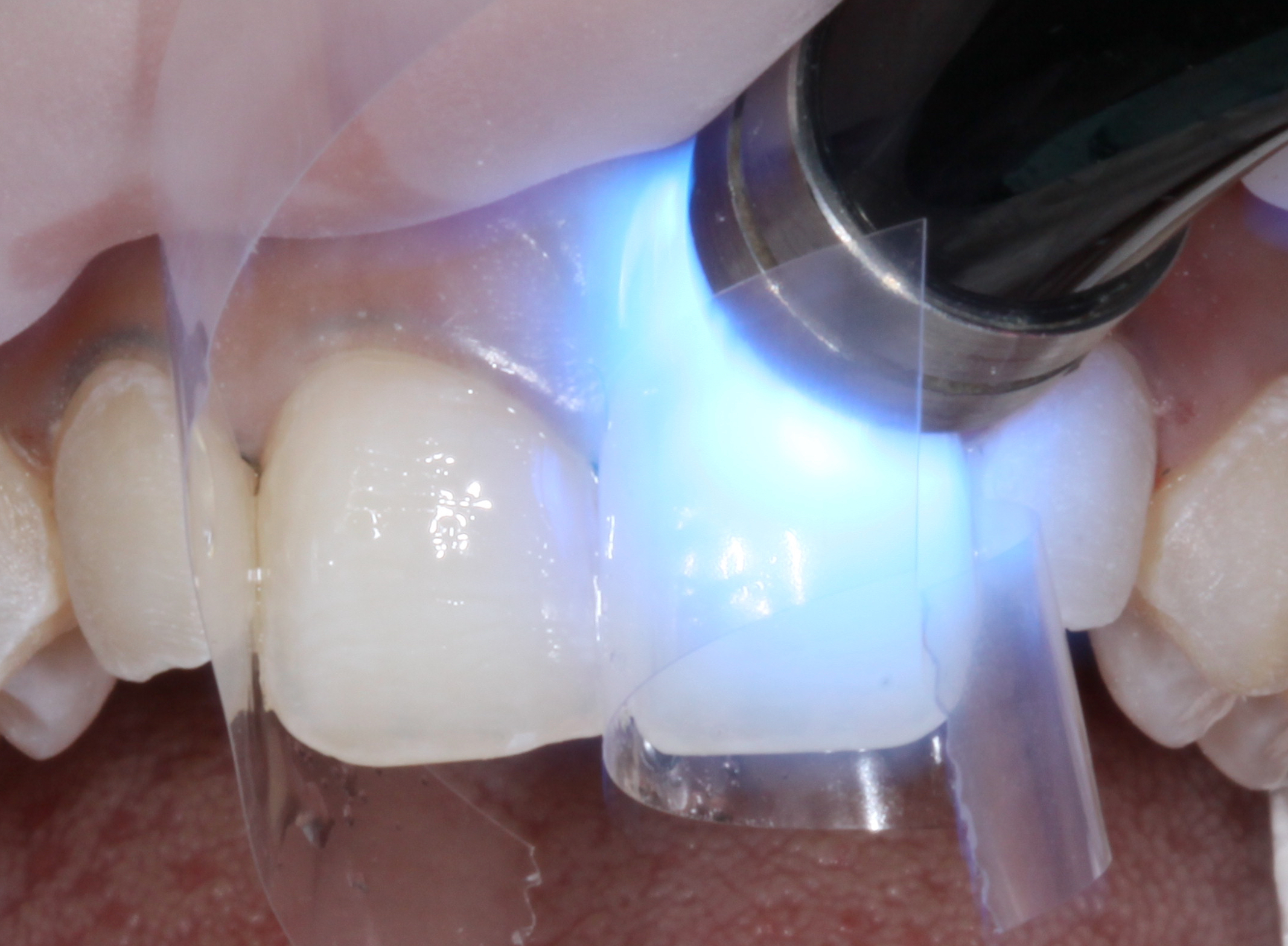
Figure 4. After the all-in-one adhesive was properly placed and light cured, the tooth surface was ready for composite resin bonding.
Next, a very thin film layer of nanohybrid composite resin (G-ænial A’CHORD A1 [GC America]) was placed along the lingual and incisal aspects of the PVS matrix of both central incisors (Figure 5). The PVS matrix was then placed on the teeth, so the composite resin material intimately adhered to the lingual aspect of both central incisors.

Figure 5. The PVS matrix was then placed on the teeth, so the composite resin material intimately adhered to the lingual aspect of both central incisors.
After light curing the composite resin, the matrix was removed, which revealed a hardened lingual and incisal halo shell. This shell mimics the position, color, and contour of the lingual enamel coloration and the incisal halo shade3,4 (Figure 6).

Figure 6a

Figure 6b – (Figure 6. After light curing, the PVS matrix was removed to reveal a thin lingual/incisal shell of composite resin.)
Next, a body shade (G-ænial Sculpt OBW [GC America]) was used to brighten the appearance of the tooth. Then a translucency for youthful teeth (G-ænial Sculpt JE [GC America]) was placed as the final layer and shaped prior to final curing. It is important to note that each layer of composite resin should be cured prior to applying the next layer. Final shaping, contouring, and polishing were completed on both central incisors.
Next, the lateral incisor and canine were done together on the left side to completion, followed by the right side (Figure 7). Once again, using the PVS matrix, the lingual and incisal contours were established for the right lateral incisor and canine using G-ænial A’CHORD A1 (Figure 8). Then, as a dentin replacement, an opacious dentin shade (G-ænial Sculpt AO-2 [GC America]) was placed as the second layer. This opacious dentin shade mimics dentin and assists in naturally blocking out any translucency.5

Figure 7. After fully sculpting the composite resin veneers on the central incisors, the left lateral incisor and canine veneers were sculpted to a semi-finished state.

Figure 8. Using the PVS matrix, the lingual and incisal contours were established for the right lateral incisor and canine using G-ænial A’CHORD A1 (GC America).
The next layer of body shade (G-ænial Sculpt OBW) was placed and sculpted onto the opacious dentin to ensure bubble-free composite resin blending. Using an interproximal carver, mamelons were artistically sculpted to mimic the internal characteristics of a natural tooth.
Each layer was light-cured prior to placing the next layer. Color modifiers, like violet and opal color tints (Kolor + Plus [Kerr Corporation]), were artistically placed along the proximal and incisal areas to create subtle incisal characterization. Once again, this was light cured (Figure 9).

Figure 9. Color modifiers like violet and opal color tints (Kolor + Plus [Kerr Corporation]) were artistically placed along the proximal and incisal areas to create subtle, natural characterization.
Finally, using a free-hand artistic sculpting technique, a youthful translucent shade (G-ænial Sculpt JE) was sculpted over the facial surfaces. This final layer was handsculpted with a flat artist’s brush (No. 4 flat brush) to create natural facial contours and mimic feminine topography.6 Final light curing was done on both the facial and lingual surfaces. To seal the surface of the composite, resin glycerin (Glycerin USP) was placed and light cured. Doing this removed the oxygen-inhibited surface layer (Figure 10).

Figure 10. It was evident that the composite resin veneers were also necessary along the premolars to bring out the buccal corridors to fill out the smile-line.
To create a full, dynamic smile and fill out the buccal corridors, the premolars were also veneered using the same sequence of bonding.
For all veneered teeth, the following sequence of finishing and polishing was done: To create primary and secondary anatomy, a medium diamond chamfer bur (850FG-016 [Komet USA]) was used to artistically sculpt along the line angles and facial surface to create the dynamic appearance desired by this patient.7 Then aesthetic contours were refined using aluminum oxide finishing discs (Sof-Lex finishing discs [3M]) and a green stone point bur (Dura-Green Stones [Shofu Dental]).
The margins were further refined with anatomical finishing burs (H50A-FG-010 [Komet USA]) and Q-Finisher finishing burs (H50AQ and H274QFG-018 [Komet USA]). A micro-diamond-infused polishing wheel (Footsies, pre-polishing-94028M.RA.130 [Komet USA] and high-shine-94028F.RA.130 [Komet USA]) was used to achieve a nice high polish for this nanohybrid composite resin. Finally, micro-diamond polishing paste (eg, 1.0 µm Diamond Polish [Ultradent Products]) was used with a buff wheel to bring out the mirror-like surface luster of this nanohybrid composite resin (Figure 11).

Figure 11a

Figure 11b – (Figure 11. Using a minimally invasive treatment procedure to treat the young cosmetic dental patient creates high-impact aesthetic results in one appointment, as seen in these before and after photos.)
Using a systematic approach, proper technique, and state-of-the-art dental materials, beautiful results can be attained in correcting cosmetic dental problems using minimally invasive techniques (Figure 12).

Figure 12. In meeting the goals of my young cosmetic dental patient, it was important to infuse the objective elements of smile design.
CONCLUSION
When treating a younger cosmetic dental patient, it is important to create the look he or she wants (Figure 13). Having a systematic approach is key to being successful with this generation. Social media plays a huge role in the life of younger patients, so understanding their goals is important to be successful with cosmetic dental treatment (Figure 14). Being able to deliver a one-appointment cosmetic restorative treatment is not only gratifying for the patient but also a good achievement for the clinician.

Figure 13. The goal of the patient to create dynamic facial beauty was met in her new smile design.

Figure 14. Social media plays an important role in the lives of the younger generation. You can see how cosmetic dentistry has changed her life for the better.
References
1. Spoor R. The use of direct composites in the conservative esthetic correction of the anterior dentition. J Cosmetic Dent. 2006;22(3):90–6.
2. Kugel G. Materials continue to expand dentistry’s options. Compend Contin Educ Dent. 2012;33(1):80.
3. Fahl N Jr. A polychromatic composite layering approach for solving a complex Class IV/direct veneer/diastema combination: Part II. Pract Proced Aesthet Dent. 2007;19(1):17-22.
4. Magne P, Holz J. Stratification of composite restorations: systematic and durable replication of natural aesthetics. Pract Periodontics Aesthet Dent. 1996;8(1):61–8; quiz 70.
5. Villarroel M, Fahl N, De Sousa AM, et al. Direct esthetic restorations based on translucency and opacity of composite resins. J Esthet Restor Dent. 2011;23(2):73-87. doi:10.1111/j.1708-8240.2010.00392.x
6. Strain R. Class IV composite repair: a heavily textured central incisor. JCD. 2014;30(1):14–9.
7. Peyton JH. Finishing and polishing techniques: direct composite resin restorations. Pract Proced Aesthet Dent. 2004;16(4):293–8; quiz 300.
ABOUT THE AUTHOR
Dr. Okuda is a past national president (2002 to 2003) and an accredited member of the American Academy of Cosmetic Dentistry (AACD). He is also a Fellow of the International College of Dentists and the International Congress of Oral Implantologists. In 2014, Dr. Okuda was proud to have achieved his Accredited Fellowship with the AACD. He is currently the aesthetic dentistry expert to the National Dental Expert Advisory Board of the AGD. He has also been the aesthetic columnist of the AGD’s General Dentistry publication for the last 8 years. He is the founder of the Pan Pacific Dental Academy (panpacdental.com).
Over the last 27 years, Dr. Okuda has been a keynote and featured speaker on cosmetic and restorative dentistry at numerous conferences and universities around the world. For the last 15 years, Dr. Okuda has been one of Dentistry Today’s Leaders in Continuing Education. He is the co-founder of the Give Back a Smile National Charitable Foundation. The foundation has provided more than $15 million in free cosmetic dental services to survivors of domestic violence for more than 20 years. He can be reached via Instagram at @panpacdental.
Disclosure: Dr. Okuda received a partial honorarium for writing this article.