Nina Lord explores the physical manifestations that can be seen in patients due to nutritional insufficiencies.
As dental professionals, we are in a fortunate position to notice changes in our patients over time. Therefore, as well as benefitting their oral health, we can have a positive effect on their wellbeing.
In this article, the physical manifestations that can be seen in patients due to nutritional insufficiencies will be discussed. This will allow you, the clinician, to have the confidence to action this when assessing and treating patients.
The starting point of this article is in the form of a case study.
Vitamin D
The thumb nails in Figure 1 belong to patient J.
J had been attending the surgery for routine care for years. At each appointment I would notice the developmental issues on his thumb nails. I suggested a visit to the GP for appropriate testing. Once it had been pointed out at a few appointments, the patient started to monitor them. They noticed that the condition of the thumb nails was declining, so an appointment was made with the GP.
The patient was referred by the GP for nail scraping. With various blood tests, it was detected that they had a very low vitamin D status.
The patient had a history of skin cancer. After digging a little deeper it was found that they had avoided sun at all costs due to the fear of getting skin cancer again. In fact, they were quite frightened at the prospect.
The doctor advised that the deficiency had manifested this way due to fact that vitamin D is necessary for the body to absorb calcium. This is needed to produce a healthy nail.
The patient was told that this deficiency could have led to osteoporosis. The same mechanism is needed for bone health.
Sunyecz (2008) concluded that: ‘Vitamin D deficiency enhances the mobilisation of calcium from the bone’ thus increasing risk of osteoporosis.
This patient took a supplement as recommended by their doctor and levels are returning to normal. The patient now reports an increase of energy and feeling of general wellbeing. They didn’t realise just how tired they were as how they felt had become their ‘normal’.
Inflammation & immunity
Vitamin D is well known for its role in general wellbeing, in particular inflammation and immunity. This was highlighted by a study by the University of Edinburgh in April 2019. Researchers found the presence of vitamin D ‘to affect key cells of the immune system’.
The reason patient J has been mentioned is because it highlights just how important noticing this development issue was for this patient. How far could this deficiency have gone? What potential impact would it have had on their health?
It also gave me (as the clinician) an insight into what the patient had gone through in the past and how they still feel about it.
This helped towards creating a wonderful relationship between the two of us – one of empathy from myself and a feeling of really being cared for by the patient.
It also highlights the importance vitamin D can have when it comes to gum health and how deficiency could be a potential risk factor for periodontal disease.
Jagelaviciene et al (2018) concluded that: ‘Vitamin D is significant in periodontology’ due to the ‘specific immune response by suppressing the destructive effect of chronic periodontitis’ alongside the role in ’jawbone density homeostasis preventing osteoporosis’.
Najeeb et al (2016) advised: ‘Clinical studies have suggested that a deficiency of vitamin D leads to periodontal inflammation and a delay in post-surgical periodontal healing’. Knowing this, could it be worth routinely liaising with GPs to have patients with periodontal disease to have their vitamin D status checked?
If vitamin D deficiency is suspected then a test is needed to provide a base line before supplementation is recommended.
Vitamin C
Vitamin C plays a huge role in the synthesis of collagen and integrity of the blood vessels. Insufficiency can manifest as small blood vessels in the floor of the mouth due to a lacking of integrity of the blood vessels (Maxfield et al, 2019).
The history of the sailors in the 18th century suffering from scurvy due to the absence of vitamin c in their diet is well known. Scurvy is a condition that leads to ‘bleeding gums and loss of teeth’ (Maxfield et al, 2019).
The blood blisters may be more noticeable in a patient who is a smoker as they use up a lot more vitamin C due to the antioxidant properties it provides (Maxfield et al, 2019) (Figure 2).
Reactive oxidative species (ROS) from leukocytes lead to destruction of periodontal tissues when in the presence of bacteria (ie, plaque) and as they are non-specific, they will harm healthy tissues too.
Najeeb and colleagues (2016) concluded in a systemic review of nutrition and periodontal health that: ‘Studies suggest that antioxidants may overcome the ROS-mediated inflammation of periodontal tissue’.
With its role in collagen production and antioxidant properties, vitamin C is a very important nutrient for periodontal health.
Varied diet
According to the NHS website, an adult needs ‘40mg of vitamin C a day’, which can be easily achieved by eating a varied diet of fruit and vegetables. Ideally, advise to your patient to eat 10 or 11 portions a day, while making them aware that vitamin C is water soluble so is therefore not stored in the body, as a result it needs to be replenished daily.
Vitamin C is found in most fruits and vegetables, and Maxwell et al (2019) advise that ‘90% of vitamin C’ is absorbed this way.
According to the National Institutes for Health (NIH), a smoker needs an additional 35mg per day, so may benefit from supplementation if they are not prepared to quit.
Magnesium
Insufficiency can manifest as a tremor, tic or twitching (DiNicolantinio et al, 2018), which can cause the tongue to quiver when at rest. This can be quite noticeable during a dental treatment as it can move the instruments, or fight the suction tube when being retracted.
Magnesium plays a vital role in the production of cellular energy, so if you notice a quivering tongue it wouldn’t cause any harm to recommend magnesium bath flakes, as magnesium is absorbed well transdermally.
Kass et al (2017) in a pilot study found ‘a rise in magnesium serum in the urine of the participants’ after being treated with a transdermal application of magnesium.
Cuciureanu and Vink (2011) provided a systematic review that concluded that ‘high stress levels are highly associated with magnesium levels’, meaning that when stressed we need more of this mineral.
Goyal et al (2013) highlighted the link between stress with system inflammation including periodontal disease. This is due to the physical factors and also psychosocial behaviours linked with feeling highly stressed. For example, poor oral hygiene, fatigue etc.
Food sources are numerous and include spinach, kale, broccoli, avocado, legumes such as kidney beans and chickpeas, banana, raspberries, salmon, mackerel, and tuna.
B vitamins
B vitamins are sometimes known as ‘the stress vitamin’. Like magnesium, we use up a lot more of these vitamins when stressed.
Young and colleagues (2019) provided a systematic review that found an increase in B vitamins either through diet or supplementation ‘improved mood’ and helped to ‘decrease anxiety in participants’.
If we don’t provide this additional need then the following conditions can occur:
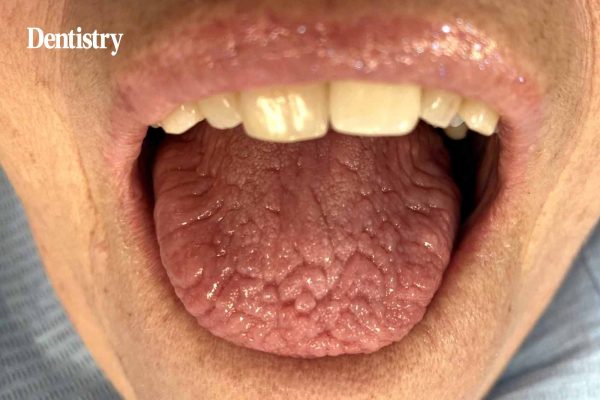
- Bilateral sores in the corners of the mouth can appear that don’t heal after a few weeks (Figure 3). This can develop into angular cheilitis in the right environment
- Cracks in the tongue, red tipped tongue and geographic tongue can all be a sign that there is a B vitamin deficiency/insufficiency (Figure 4).
Glossitis, also known as ‘red beefy tongue’, was described as ‘a useful tool to diagnosis B12 deficiency’ by Zhoul et al (2018) (Figure 5). They concluded that: ‘Physicians should pay special attention to oral manifestations during physical examination in high-risk populations such as the elderly, vegetarians, and patients with digestive problems.’
The study also advised that deficiency can lead to neurological problems later in life. While Miranti et al (2017) advised of link between B vitamin deficiency and gastric cancer.
Seeing the GP
So, by noticing this and auctioning a GP referral, you could prevent a serious health issue in your patient.
B vitamins are synthesised and absorbed in the small intestine. If your patient has digestion/absorption issues, supplementation may not help them. They may struggle to absorb them and will only provide them with what my nutrition teacher explained in the classroom as ‘expensive urine’.
If the patient has digestive issues, they need to see their GP and/or nutritionist/dietician to help them with this. Supplementation may be needed in the form of an injection, which will bypass the digestive system.
Action to take here would be to refer to GP.
B vitamins can be found in most food sources. This includes meats, seafood, dairy such as cheese and milk, dark leafy vegetable, beans and legumes.
Essential fatty acids/omega 3
The National Institutes of Health describes the most common sign of deficiency as ‘rough, scaly skin and dermatitis’. This can be noticed as dry flaky lips or flaky skin under the eyes.
One of the reasons omega 3 is so important is because of the anti-inflammatory effect it has on the body.
However, in modern diets, a lot of our patients eat more omega 6 foods. They are usually processed foods rich in vegetable oils. This is problematic, as omega 6 has a pro-inflammatory effect in the body.
Hibbeln et al (2014) discussed the importance of the omega 3:6 ratio. If more omega 6 is consumed than omega 3 this ‘leads to a tilt toward inflammatory processes in the body’.
Simopoulos (2002) concluded in a literature review that a beneficial ratio of 2/3 of omega three to one on omega 6 suppresses inflammation’
Recommend your patients eat oily fish two or three times a week. Advice reducing foods containing hydrogenated vegetable oils to help them to achieve this balance.
Zinc
According to Pisano and Hilas (2016): ‘Zinc deficiency may lead to loss of appetite, impaired immune function, weight loss, delayed healing of wounds, eye and skin lesions, and smell and taste disturbances’.
There may not be a physical manifestation present. However, a patient will often talk about a bad taste or even lack of taste with the clinician.
Ozler et al (2014) advised that: ‘The findings suggest a relationship with zinc deficiency and recurrent aphthous stomatitis’. Suggesting frequent oral ulceration could be connected to zinc deficiency.
Food sources include lamb, shellfish, nuts, seeds, legumes and eggs.
Take-home messages
Always go from a food first perspective. Advise a wide and varied diet to avoid the deficiencies mentioned in this article. This includes:
- Oily fish two or three times a week, while avoiding hydrogenated vegetable fats to achieve omega 3:6 ratio
- 10-11 portions of fruit and vegetables a day
- Six to eight glasses of water per day.
- Do not supplement blindly as there may be an underlying issue affecting absorption. Green pharmacy can provide side effects too. Everyone has their own individual needs, not to mention the risk of drug interactions.
- The ability to use an inner detective when noticing conditions. Are there a few symptoms combined which tells the clinician something about the patient? If a patient has a cracked and quivering tongue this could highlight that the patient is highly stressed or fatigued. Asking them how they are in themselves might mean they open up. They may give an insight as to what is affecting their motivation with routine.
- Refer to the appropriate person if the patient can benefit from this and they are open to it. It really does take a village when caring for patients and it is very important to work within scope. Connect with people who can be referred to. Create an inner circle of like-minded people to provide the best care for the patient. This can be the patient’s GP, a local nutritionist/dietician or any other healthcare professional who is relevant to the patient.
Further reading
Omega-3 fatty acids fact sheet, from the National Institutes of Health, Office of Dietary Supplements: ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional
Vitamin C fact sheet, from the National Institutes of Health, Office of Dietary Supplements: ods.od.nih.gov/factsheets/VitaminC-HealthProfessional
The Eatwell Guide from the NHS: www.nhs.uk/live-well/eat-well/the-eatwell-guide
Like this article? Sign up to Clinical Dentistry magazine here.