Amazing Technology
The medical management of gangrene during the American Civil War was to amputate a limb above the infection site to prevent ongoing bacterial proliferation into the surrounding tissues. (Fig. 1)
Fig. 1

170 years ago, the medical model for treating gangrene was to amputate a limb above the infection.
During a lecture in 2000, Dr Graham Mount, a pioneer in the clinical use of glass ionomer cement, described dentistry as “the only health care profession that still treats an infectious disease by amputation.”
In the last few years, dental technology has made significant advances to facilitate the diagnosis and replacement of tooth structure by either partial or complete amputation of teeth.
Sadly, all this amazing technology remains based upon the principles of the medical management of infectious diseases practiced over 150 years ago. This is especially unfortunate when there are so many more conservative treatment options currently available.
The Medical Management of Infection
Dental caries is a bacterial infection of tooth structure caused by changing circumstances within the oral environment. There are defence mechanisms in the dentin pulp complex, that are capable of slowing or reversing the rate of caries proliferation.
Arrested caries are an example of how, in a favourable oral environment, teeth are able to remineralize caries infected dentine. (Fig. 2)
Fig. 2
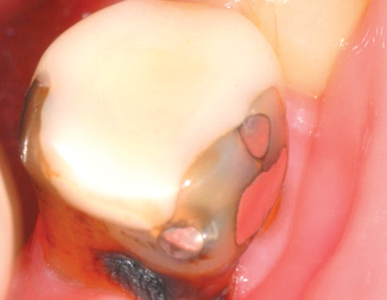
Arrested caries demonstrates a tooth’s ability to remineralize caries into dental scar tissue.
As the collagen matrix within the dentin has been denatured by the carious process, normal dentin is unable to form, and remineralization occurs by the deposition of mineral salts from the dentinal tubules and saliva. The dark colour of arrested caries is due to the inclusion of sulphur ions into the remineralizing tissues.
Arrested caries can be compared to scar tissue, where the dermis is unable to reform, so a protective layer of scar tissue (arrested caries) is laid down to cover the wound area to prevent bacterial incursion into the tissues beneath.
The Medical management of Caries
The current medical management of a dermal infection is to:
- Clean the wound.
- Place a medicament to enhance the natural healing process.
- Isolate the infected site from a hostile environment and enable the healing process to occur.
These same principles can be applied to the management of dental caries.
Clean the wound
Carious dentin contains a high degree of surface bioload consisting of bacterial plaque and other debris present within the mouth. Infected surface dentin may be so badly broken down that it splits away from the surface of the caries.
Within the carious dentinal tubules, necrotic debris and bacteria are present that can interfere with the healing process.
Surface preparation consists of removing badly broken-down infected dentin and the bioload from the surface of the caries and into the infected dentinal tubules.
Broken down infected dentin can be removed with a small excavator, gently levering it from the surface of the caries.
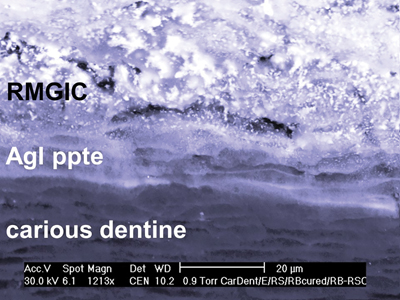
Bioload can be efficiently removed, to facilitate penetration of medicaments from the surface of the caries and into the dentinal tubules, by the application of 37% phosphoric acid for 15 seconds, washing with water and gently air drying. Polyacrylic acid will not remove bioload from the dentinal tubules. (Fig. 3)
Fig. 3

This demonstrates how effective etching is at removing necrotic tissue and bioload from non vital dentinal tubules enhancing both the penetration of medicaments and RMGIC as shown. Poly acrylic acid conditioning does not.
Apply a medicament to enhance healing (remineralization).
Fluoride release from glass ionomer cement has a limited effect in arresting caries and has been used extensively for caries management in remote communities (Atraumatic Restorative Treatment), however GIC cannot be relied upon for total caries management and requires additional pharmacological assistance to be truly effective.
Ozone gas has been used as an effective caries management tool, but its use is limited due to the lack of an efficient delivery system.
Fluoride varnish application has been shown to have limited clinical benefit.
Silver fluoride compounds are highly bactericidal and have long been used to arrest caries; silver nitrate has been used since the early 1900s, and silver diamine fluoride was identified from Japanese literature for arresting caries in the early 1970s. Fig. 4 shows the bactericidal effects of AgI deposits on a carious dentin surface.
Fig. 4
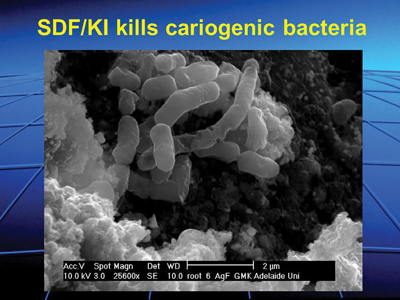
Shows the bactericidal effect of AgI deposited on the surface of carious dentin after SDF/KI treatment.
Aqueous silver fluoride (AgF) and silver diamine fluoride (SDF) both effectively arrest dental caries. However, the side effect of staining the arrested caries black has generally limited their use for the management of caries in deciduous teeth and root caries.
Staining by AgF and SDF can largely be prevented by the immediate application of potassium iodide (KI) that scavenges any remaining free silver ions to form silver iodide, a creamy coloured white precipitate. Fig. 5 shows the difference in staining of a GIC restoration when one cavity was treated with SDF and the other with SDF/KI.
Fig. 5

Demonstrates the effectiveness of SDF/KI in preventing staining compared to SDF alone.
The application of potassium iodide during pregnancy or patients with thyroid issues should be done in consultation with an appropriate medical practitioner.
Isolate the infection from the environment to improve healing (remineralization)
Composite resin is a popular material for the replacement of lost tooth structure and is an excellent restorative material for cavities caused by a lost restoration without residual caries or tooth loss caused by trauma.
Composite resin relies upon the bond of resin based dental adhesives that adhere poorly to caries affected and infected dentin. In order to repair a carious lesion with composite resin, all remaining caries must be removed prior to bonding onto sound dentin, and this requires the removal of a lot of remineralized tissue. In essence, composite resin is unsuitable as a restorative material to restore carious teeth.
Glass ionomer cement has a weak chemical bond to sound and carious enamel and dentin. As the interface between a tooth and glass ionomer cement is stress free, high bond strengths are not required. Furthermore, prior application of SDF and AgF enhances the bond strength of GICs to enamel and dentin. (Fig. 6)
Fig. 6
The application of SDF/KI to carious dentin increases the bond strength between caries and resin modified GIC.
High strength GICs are indicated for single surface restorations where there are no unsupported cusps present. These include occlusal surfaces, proximal surfaces using tunnel or slot preparations and lesions at the gingival margins.
- Figures 7 to 9 show a clinical restorative procedure using the medical model of caries management:
- Figure 7: A cavity is prepared for a
silver fluoride treated restoration, leaving significant caries in situ. - Figure 8: Shows the cavity following a 15 second etch and SDF/KI placement. Notice the white precipitate of AgI on the surface of the carious dentin.
- Figure 9: Shows the completed restoration.
Fig. 7

An occlusal cavity preparation with supported cusps for the restoration of caries prior to SDF/KI and a GIC overlay.
Fig. 8

Following a 15 second etch, the caries has been treated with SDF and KI. Notice the white precipitate of AgI on the caries surface.
Fig. 9

A wear resistant GIC restoration provides a simple and predictable solution for the management of single surface caries.
Multi surface restorations require the extra strength of a composite resin overlay over the GIC base, or a conservatively prepared indirect restoration.
In summary, single surface restorations to remineralize caries are placed as follows:
- Remove excessive bioload with a small excavator
- Etch for 15 seconds, wash, and dry the preparation
- Apply one or two drops of SDF or AgF onto the caries, avoiding gingival tissues.
- Immediately apply KI until the white precipitate becomes clear
- Wash away reactant and air dry
- Place a GIC restoration.
The placement of a multiple surface restoration follows the same steps using a Resin modified GIC (RMGIC) instead of auto cure GIC, as a base or liner, prior to placing a composite resin or indirect restoration overlay.
Figure 10 shows the remineralization ability of SDF/KI on an asymptomatic carious lesion14 months after placement and Figure 11 shows how the use of SDF/KI prevented SDF staining of the restoration over that time.
Fig. 10

Large asymptomatic caries on multiple surface cavities shows the healing (remineralizing) ability of a SMART GIC, composite resin sandwich restoration.
Fig. 11
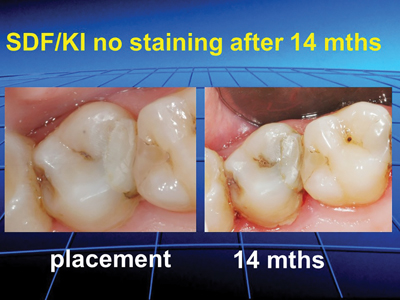
A large multi surface SMART restoration treated with SDF/KI eliminates staining at the cavo margins.
Fig. 12

Author’s book which presents evidence-based research for applying the current medical model to restorative dentistry with appropriate restorative procedures described in depth for each clinical situation.

QR code opens the author’s book web site on Amazon.
Opportunities
In many ways the dental profession is at a crossroads.
The delivery of high-tech treatment offers patients choices that would otherwise be unavailable to them. Unfortunately, such procedures are often highly invasive, time-based treatments that do not provide permanent solutions to patient needs and have cost constraints that limit their availability. Furthermore, the enthusiasm amongst the dental profession to adopt these technologies can lead to over diagnosis and prescription of their use.
Within this mix of the treatment options available to dentists, there are clinical situations to treat carious teeth, that would be better managed by using a more conservative medical based model of care.
Medical caries management is based upon the treatment protocols of Atraumatic Restorative Treatment (ART) that has been successfully used to treat caries in both established and emerging economies for a number of years. The enhancement of ART by the application of silver-based medicaments creates the interesting acronym; Silver Modified ART or SMART.
SMART is a treatment model of care that:
- Enables high quality and predictable dental restorations over a wide range of platforms in established and emerging economies
- Provides a virtually pain free and relaxed environment for both patients and dentists that encourages the super efficient delivery of care.
- Dramatically reduces the need for general anaesthetics for asymptomatic and apprehensive children
- Lays the ground for future minimally invasive management of dental caries
By leaving caries in situ, SMART enables the predictable, efficient and stress-free delivery of restorative care with benefits to both patients and clinicians and can be readily accessible on a global scale.
In reality, the coexistence of SMART and high-tech dentistry offers patients the very best of care across a wide range of treatment modalities and lays the foundations for the successful evolution of the profession.
Oral Health welcomes this original article.
About the Author
 Geoff Knight is a general dentist from Melbourne, Australia. He is an internationally recognized dental speaker with a focus on preservation dentistry and has published a book on this topic: SILVER FLUORIDE AND GLASS IONOMER CEMENT: A SMART Operative Guide for Working with Teeth. The book presents evidence-based research for applying the current medical model to restorative dentistry with restorative procedures described in depth for each clinical situation.
Geoff Knight is a general dentist from Melbourne, Australia. He is an internationally recognized dental speaker with a focus on preservation dentistry and has published a book on this topic: SILVER FLUORIDE AND GLASS IONOMER CEMENT: A SMART Operative Guide for Working with Teeth. The book presents evidence-based research for applying the current medical model to restorative dentistry with restorative procedures described in depth for each clinical situation.
Read more from the 2022 Preventive Dentistry issue.


