We prospectively included 22 patients—seven males and fifteen females, mean age 26 (range 18–43)—undergoing orthognathic bimaxillary surgery at the Oral and Maxillofacial Surgery Unit of Sant’Orsola-Malpighi University Hospital (Bologna, Italy) between July 2017 and June 2019. Eight patients were diagnosed with skeletal class 2 deformity (one with combined facial asymmetry), ten were diagnosed with skeletal class 3 (six with combined asymmetry), three patients were diagnosed with class 1 facial asymmetry and one with anterior open bite. The present protocol was approved by the Sant’Orsola-Malpighi University Hospital ethics committee (approval number 238/2012/0/Disp PL02, amended 18/10/2016); the study conformed to the principles of the Declaration of Helsinki. Informed consent was obtained from all patients upon enrollment in the trial.
The study workflow consisted in the following steps: (1) data acquisition, (2) virtual planning, (3) computer-aided design and 3D printing of customized positioning guides and implants, (4) surgery and (5) Outcome evaluation.
Data acquisition
Patients were enrolled when pre-operative orthodontic treatment was completed or when an adequate and stable final occlusion was achieved. All patients performed a pre-operative CBCT-scan (NewTom VGI Evo—Cefla Group, Imola, Italy), (24 × 19 cm FOV, 0.3 mm voxel) in a clinically-determined natural head position (NHP) and using a wax bite obtained in clinically-set condylar centric relation (with the aid of Dawson’s maneuver), 1 month prior to surgery.
Dental digital models were acquired using the CS 3600 intraoral scanner (Carestream Health Inc, Rochester, NY, USA) to produce stereolithographic output files (.STL) and obtain a virtual model of the dental arches. Digital models were 3D-printed using a stereolithographic printer (Form 2, Formlabs Inc., Somerville, MA, USA) and the final occlusion was manually determined. Models in final occlusion were re-scanned obtaining the corresponding digital model (.STL format).
Virtual planning
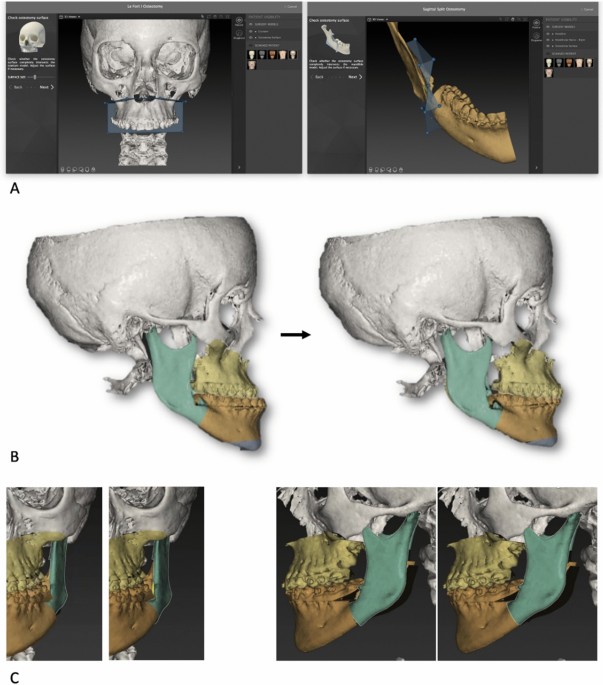
Cone-beam CT datasets (exported in DICOM format) and data from the intraoral scans were processed by the surgeon using IPS Case Designer software (KLS Martin, Tuttlingen, Germany). This software allowed to segment patient’s facial hard tissue and register dental digital models on the DICOM-segmented mesh with a semi-automatic algorithm. Moreover, it allowed to perform a three-dimensional cephalometric analysis, according to Swennen11, virtual BSSO was designed in order to replicate the expected achievable osteotomy (Fig. 1A). The surgical team realised the virtual surgical planning according to aesthetic parameters and cephalometric measurements (Fig. 1B). This allowed to plan the condyle/ramus fragment adjustments (Fig. 1C) pivoted on the geometrical center of the condylar head, with the following goals: (1) avoiding interference with the teeth-bearing fragment or (2) knowing unavoidable interference to be managed with selective additional osteotomies of the lingual fragment, (3) aligning the inferior borders on the sagittal plane; (4) obtaining the least possible condylar displacement compatible with the requested ramus adjustments. A couple of surgical splints (intermediate and final) was designed based on the virtual surgical plan. The mandibular procedure was designed as a potentially splint-less surgery, nevertheless surgical splints were produced in order to have a back-up solution in case of intraoperative failure of the system. Eventually, the intermediate splint was systematically used in order to keep the teeth-bearing fragment more stable during fixation.
(A) Virtual osteotomies in IPS CaseDesigner. (B) Virtual surgery planning in IPS CaseDesigner. (C) Ramus position planning in IPS CaseDesigner. Single images joined in Adobe Photoshop 19 software (Adobe Inc. San Jose, CA, U.S.).
PSIs and positioning guides design and manufacture
The surgical plan was uploaded as a proprietary format (.ips for the planning, .spl for the splints) to the technical service through the IPS Gate web platform (KLS Martin, Tuttlingen, Germany). The original datasets (CBCT scan and digital models) were also uploaded. Subsequently, KLS Martin technical service designed the individualized mandible positioning guides, patient-specific plates and splints under the guidance of the surgeon. The positioning guides were designed to precisely guide the buccal and sagittal osteotomies, and the level of the lingual osteotomy, in order to reproduce the mutual relationship between the bony fragments according the points listed in the previous paragraph; screw trajectories were planned in order to avoid teeth roots and the inferior alveolar nerve (Fig. 2C). Three guide designs were used throughout the trial (Fig. 2A, B): Design A was built from selective laser sintered (SLS) polyamide, and was composed of a mandibular shell with a groove for the vertical osteotomy and a groove for the sagittal osteotomy; an inferior hook for the inferior border; holes for screw fixation of the guide (1.5 mm) and transfer of the custom-made plates (2.0 mm); an arm for teeth reference on the occlusal surface of the last two dental elements of the patient’s arch, in order to maximize accuracy and stability of the guide during surgery. Design B was analogous to design A except for the introduction of 7 mm long stainless-steel sleeves in transfer holes and the trimming of the most lingual part of the shell. Design C guides were made of direct metal laser sintered (DMLS) titanium alloy (Ti6Al4V), replacing the solid shell with a triangle mesh. The dental reference was replaced by a hook which came to an anterior stop against the last or second to last tooth of the patient’s dental arch; a detailed dental reference was avoided in this design due to possible guide inapplicability, production cost and time increase, and to limit the contact between titanium and teeth enamel. The custom titanium plates were designed to reposition the proximal and distal mandibular fragments in their planned positions, using the previously drilled holes (2.0 mm) for screw fixation as a reference. Plates were manufactured using titanium alloy (Ti6Al4V) Direct Metal Laser Sintering (DLMS) 3D printing (Fig. 2D); splints were manufactured using 3D printed dental resin. Digital three-dimensional models of bony fragments and plates were also provided by KLS Martin (in .STL format).
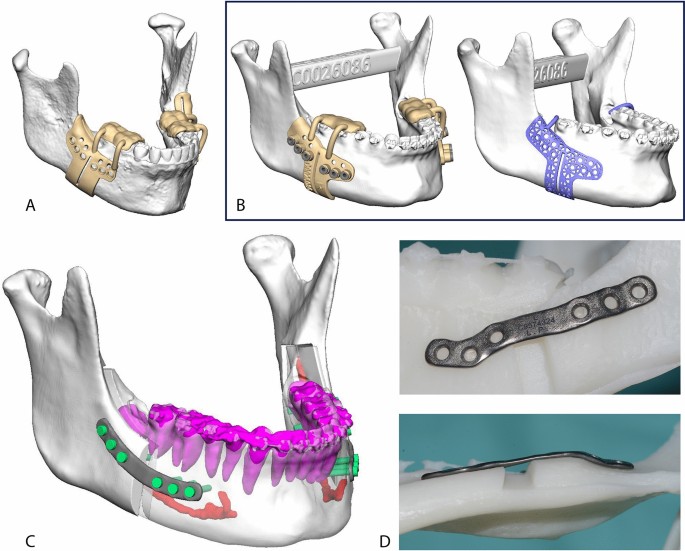
(A) Design A guide CAD rendering. (B) Design B and C guides CAD rendering. Both guide designs were produced and used on the last 10 patients. (C) Plates CAD rendering. Teeth roots and inferior alveolar nerves were segmented and carefully avoided while planning the plates’ position. (D) Plate shown on a stereolithographic model of the planned mandibular anatomy. DMLS manufacturing allows for odd shaped plates. In this case the shape was designed to avoid interferences with the mental nerve. Single images joined in Adobe Photoshop.
Surgery
All patients were operated by the first author (GB) through a mandible-first approach, using the individualized system (Fig. 3). The bony surface of the mandible was exposed according to the conventional vestibular incision to perform BSSO. The guide was secured to the mandible with two titanium screws using the designed fixation holes (1.5 mm) to avoid any mobilization during the osteotomy. With the guide in place, the surgeon marked the osteotomy lines using ultrasonic bone-cutting tools (Piezo-Surgery, Mectron SpA, Cerasco, Italy) and drilled the transfer holes for the plate using an Angulus2 angulated drill (KLS Martin, Tuttlingen, Germany). Then the guide was removed to complete the osteotomy. Eventually, the proximal and distal fragments were fixed in the planned position using the patient-specific plates under the guide of pre-drilled transfer holes (2.0 mm). The intermediate CAD/CAM splint was used to maximize the stability of the teeth-bearing fragment while performing the osteosynthesis. The upper maxilla was managed according to the best vertical position and fixed using standard titanium manually bent miniplates and screws under the guide of the final CAD/CAM splint.
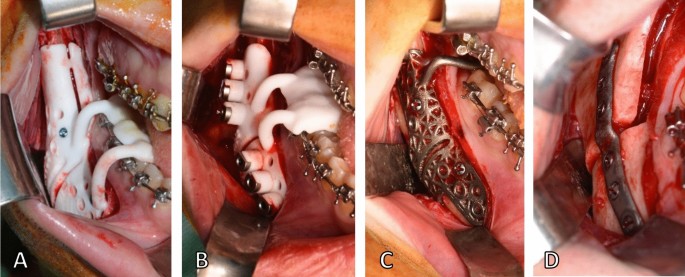
Intraoperative view of design A guide (A), design B guide (B), design C guide (C) and plate (D). Single images joined in Adobe Photoshop.
Design A guides were used on both sides of the mandible for the first 12 patients. For the last ten patients Design B and C guides were used following a split mouth procedure, using opposite guide designs on the same side for consecutive cases; once osteotomy lines were traced and screw holes were drilled under one guide type, the guide was removed and an analogous guide of opposite design was applied to cross-check holes and osteotomy lines alignment.
Intraoperative failures and complications were also assessed.
Outcome evaluation
All patients underwent post-operative imaging with a CBCT-scan 1 month after surgery, before post-operative orthodontic treatment started and any tooth movements occurred (due to rigid orthodontics and daily use of the final splint), using the same machine and parameters of the pre-operative scan and maintaining the occlusion at maximum intercuspation. The post-operative DICOM dataset was processed to obtain a 3D model of the post-operative skull, mandible and mandibular plates with the software DICOM to Print (3D Systems, Rock Hill, SC, USA) and exported in STL format. In this early trial we focused on the mandible. Planned and post-operative meshes were compared using the open source CloudCompare software (CloudCompare Project, cloudcompare.org): the teeth-bearing fragments were registered with an iterative closest point (ICP) alignment method (Fig. 4A), and subsequently visually inspected via generation of colorimetric surface maps to check the alignment (Fig. 4B). We then evaluated the discrepancy between planned and obtained post-operative position of the mandibular plates and rami by analyzing the discrepancies in terms of rotation (roll, pitch and yaw) and translation (antero-posterior, lateral and vertical). These movements were determined by incorporating the segments in homologous bounding-boxes, aligning the planned model to the post-op result via ICP alignment and colorimetric map inspection (Fig. 4C, D), then evaluating the translational shift of the geometrical center and the rotational shift of the model according to Euler angles convention. The signed discrepancies were considered and tabulated according to the patient’s side (right or left) applying a mediolateral convention. Positive signed values identify forward, upward and lateral translations; a positive pitch angle identifies a clockwise rotation as seen from the patient’s right lateral aspect; a positive roll angle identifies a lateral displacement of the caudal margin of the ramus; a positive yaw angle indicates a lateral displacement of the anterior margin of the ramus. This convention allowed for comparison between opposite mandibular sides.
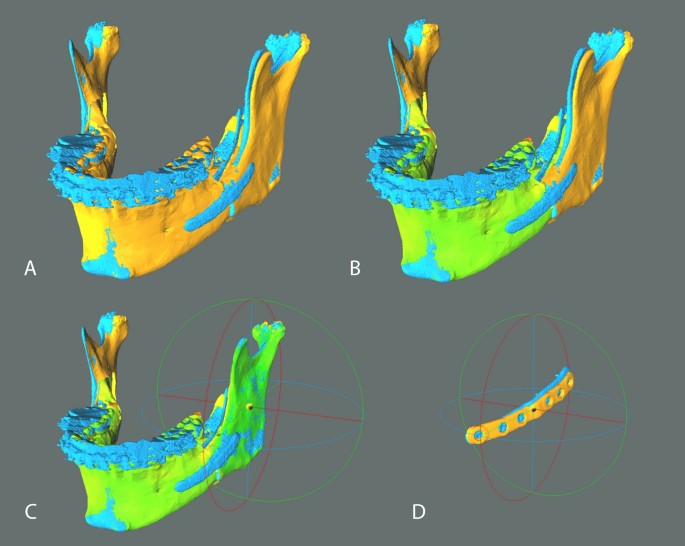
Analysis method in CloudCompare v2.9.1 software. Planned models (orange) were aligned to postoperative models (blue) on the basis of the teeth-bearing fragment (A). Colorimetric surface maps were used to check the alignment (B). Planned rami were aligned to postoperative rami position and the transformation was recorded; the alignment was visually checked via generation of colorimetric surface maps; axes and planes are also shown (X = red, Y = green, Z = blue) (C). An analogous protocol was applied to PSIs (D). Single images joined in Adobe Photoshop.
To obtain a comprehensive description of the angular and translational displacement of each 3D model considered, two further parameters were defined: total angular error and total translational error. The first is the angle in the axis-angle representation of a rigid body transformation, while the second is the translation vector module. Both measures are always positive by definition and were used to avoid positive and negative displacements canceling each other on average in the description of displacement.
The same protocol was applied to compare the preoperative CBCT-scan and the planned model, in order to quantify the planned three-dimensional shift for each mandibular ramus in respect to the pre-operative position. To accomplish this evaluation, the ICP alignment was carried out referring to the cranial base as fixed reference.
Post-operative failures and complications were also assessed.
Statistical analyses
Given the limited sample size (n = 44), all measures were summarized using median and interquartile range (IQR). However, to allow comparison with the existing literature, mean and standard deviation were also provided for each measure. Boxplots were used to display the frequency distribution of the measures. Non-parametric two-tailed tests were used in all cases due to limited sample size and theoretical asymmetric distribution of total angular and translational errors.
Because in a preliminary analysis (Mann–Whitney U-Test) performed on the first 12 patients no significant difference was found in the precision of rami and plate positioning between the left and right sides, rami and plates were considered as separate entities, without reference to the side.
Spearman’s correlation coefficient (n = 44) was used to examine the extent to which inaccuracies in the final position of the plate were associated with inaccuracies in the position of the ramus. Similarly, the correlation between the pre-operative to planned rami transformations and the inaccuracy in the final position of the rami was investigated, in order to determine whether greater planned displacements could increase the inaccuracy of the outcome.
Kruskal–Wallis test (n = 44) followed by post-hoc pairwise comparisons was carried out to analyse differences in the post-operative position of rami and plates among guide designs.
IBM SPSS Statistics 25 (IBM Corp., Armonk, NY, USA) was used to perform the analyses. For all tests the significance level was set to α = 0.05.