The adult patient with deep anterior overbite and extensive anterior tooth wear is especially challenging. Treatment involves many diagnostic questions to which correct answers must be found to ensure successful management and treatment. This type of case is a perplexing problem – how does a clinician manage restorative treatment? Today a multitude of digital diagnostic tools are available to the clinician to enhance diagnosis, treatment planning, sequencing and communicating complex cases like these.
A case treated with an interdisciplinary approach of orthodontics, orthognathic surgery and conservative restorative dentistry will be used to demonstrate the diagnostic principles including virtual smile design, treatment decisions and sequence. A fifteen-year follow-up will demonstrate the stability.
Patient History:
A referring dentist was concerned about the extensive wear of his patient’s maxillary and mandibular teeth (Fig. 1). In addition, the dentist felt that the patient had an unfavorable angle of the maxillary central incisors which were retroclined and retrusive. The patient felt like his maxillary lateral incisors were too protrusive- a common, but incorrect, observation by patients exhibiting this particular type of malocclusion. The malocclusion presented a dilemma for the dentist. In order to restore the worn and short anterior teeth, there were two options that were exclusively restorative:
- Crown lengthening of the short/worn teeth followed by full coverage restorations that necessitated significant tooth reduction.
- Opening the vertical through restoration of most of the posterior teeth in order to create restorative space anteriorly.
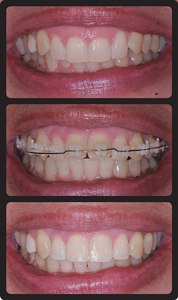
Fig. 1
Pretreatment malocclusion.
Was there another option? The problem for the restorative dentist was insufficient interocclusal space to restore the anterior teeth without significant natural tooth reduction. Compensatory eruption of the anterior teeth secondary to incisal wear is typical with these types of cases. Orthodontic intrusion of the maxillary and/or mandibular incisors could recreate the interocclusal space needed for the restoration of the worn anterior teeth with the added benefit of optimizing the gingival margins of these teeth.
The Cause of the Overbite:
a) Incisal Edge to Occlusal Plane
The occlusal plane located from connecting the occlusal contact point of the maxillary and mandibular second molars to the level of the upper lip at rest is a good reference from which to decide if anterior teeth require intrusion.1 The relationship between the maxillary and mandibular second molars cannot be changed. Restorative dentists often still request orthodontists to open the vertical dimension by extruding maxillary and/or mandibular molars in non- growing patients. This intervention is rarely stable in adults because the muscles of mastication do not have the capacity to stretch; the vertical dimension usually goes back to its original level. In growing patients, this accommodation may appear to be what occurs when correcting deep overbites, but what is actually occurring is elongation of the ramus secondary to condylar growth. While skeletal growth is happening, posterior teeth erupt to fill the space created by ramus growth.
The maxillary incisal edge should be around 3mm from the occlusal plane – a distance that decreases with age because of upper lip elongation. It is not uncommon to see the disappearance of the incisal edge of the maxillary teeth with the lips at rest in an older patient.
For the patient presented, the maxillary incisor was 4mm below the occlusal plane. Given that there was dentin visible and a normal sulcus depth, there must have been at least 2 mm of incisal wear. On average, the height of a maxillary central incisor is 10-11mm. A pleasing width-length ratio is 75% to 80%.2 The 2 mm of wear present on this patient had resulted in an unappealing width-length ratio of greater than 85%. This was factored into his overall treatment plan.
For this patient, the mandibular incisal edges, which should be at the level of the occlusal plane, were 3mm above it and also had wear. Given the supraeruption of both the maxillary and mandibular incisors, the patient would benefit from intrusion of these teeth – 3mm for the maxillary incisor and 4 mm for the mandibular incisors. Doing so would leave an anterior openbite of 1mm giving enough interocclusal clearance for the restoration of the incisors. (Fig. 2) The maxillary central incisors and mandibular incisors would require 2 to 2.5mm and 1 to 1.5mm added,
respectively.
Fig. 2

Vertical discrepancy correction with orthodontic intrusion.
b) Angulation of Maxillary Central Incisors
Traditional Cephalometrics has limitations in that appealing facial proportions can exist is a wide range of cephalometric values.3 It is important the maxillary incisors are considered part of the face and have positions that add balance to the face in all dimensions for optimal esthetics. Ideally, the maxillary central incisor should be positioned anterior/posterior where it is approximately in the same vertical plane as the forehead.4
Dr. Frank Spear advocates another mechanism to evaluate central incisor angulation: the position of the incisal third of the maxillary central incisor is usually at a right angle to the maxillary posterior occlusal plane. In the case shown this angle was obtuse (much greater than 90-degrees), reflecting a retrusive and retroclined incisal third.
This patient had retrusive maxillary central incisors which were significantly worn (Fig. 1). Retrusive incisors can contribute to a restricted envelope of function and excessive wear. As wear occurs, there is compensatory eruption. This amount of tooth wear is not from normal chewing function regardless of diet.
c) Imbalance of Facial Proportions
A disproportionate facial balance can contribute to a deep bite. The ratio of the upper facial height to the lower facial height is important to consider. The upper facial height is measured from the glabella (a region at the base of forehead) to a point just below the nose. The lower facial height is measured from a point below the nose to a point just under the chin. A proportion of 45% to 55% (upper face height to lower face height) is considered to be normal and balanced. The presenting patient had a proportionately shorter lower face height with proportions being 55% to 45% (Fig. 3). This contributed to the deep overbite. If one of the goals of orthodontic treatment was to enhance the patient’s esthetics and facial proportions, a mandibular advancement, accomplished through surgery, was indicated. In other words, once the ideal horizontal and vertical position of the maxillary dentition was achieved through orthodontic tooth movement, the full extent of the Class II skeletal relation would be unmasked, showing buccal segment relations with 8 to 9 mm overjet. Given that this patient was not growing, surgery was the only option to properly correct the Class II horizontal discrepancy.
Fig. 3

Upper face height (UFH) to lower face height (LFH) ratio.
The mandibular advancement surgery also accomplished downward or clockwise rotation of the mandible increasing the anterior vertical dimension and hence the lower face height, while maintaining the posterior vertical dimension (Fig. 10).
Virtual Smile Design:
Digital Smile Design (DSD)5,6 is fundamentally a technical tool used to model the end result of treatment. A patient’s smile is modelled digitally so that both patient and doctor can physically see the end result of treatment prior to any physical intervention. This technique is valuable in aesthetically shaping the smile and involving the patient in such a design process. DSD allows the smile to attain visually appealing portions described in subsequent sections.
In an ideal arrangement, the maxillary central incisors should provide esthetic dominance. They should be equal in length and each one longer than wide with an optimal width-length ratio of 75-80%. The lateral incisors should be shorter by 0.25 to 0.5mm. The gingival margins of the maxillary anterior teeth ideally trace a “high-low-high” outline from central incisor to canine with the lateral incisor gingival margin located more incisally. The progression of the gingival margins is considered to be normal when the gingival margin of the lateral incisor is 1.0 to 1.5mm coronal to the tangent drawn between the gingival margins of the central incisor and canine on each side. 7(Fig. 4B).
Fig. 4A,B

Virtual smile design.
The maxillary central incisors are approximately the same length as the canines with their gingival margins being at the same level. This arrangement results in what Sarver8 refers to as “smile arc” (Fig. 5) wherein the curvature formed by the incisal edges of the maxillary incisors and canines is parallel to the curvature of the lower lip in a posed smile.
Fig. 5

Non consonant (flat) and Consonant Smile Arc.
When the maxillary incisors are over-erupted, as can occur in the presence of a restrictive envelope of function or a protrusive bruxing habit, shortened central incisors can result. Orthodontic intrusion of the short teeth should be followed by restoration of the incisal edges to improve the incisor crown lengths and proportions.
If a patient has gingival display on smiling, discrepancies in crown heights are unaesthetic and can be corrected with gingival surgery, extrusion and equilibration of the longer incisor, or orthodontic intrusion and restoration. The proper treatment is determined based on the sulcus depth, incisal wear and the relative crown lengths of the central and lateral incisors. It has been observed that the most common crown discrepancy when treating adults is over eruption and compensatory wear of the central incisor(s). (Fig. 1).
If both central incisors are worn (Fig. 6) they can be orthodontically intruded simultaneously to achieve vertical clearance for temporary composite incisal restorations. If required this is restored more permanently with a porcelain crown or veneer. As a tooth is intruded, the gingival margins migrate apically the same amount as the tooth9 indicating that the patient’s biologic width is maintained despite the intrusive movement. An important concept to understand is that the clinical crowns do not become shorter as the roots are intruded into the bone.
Fig. 6
Orthodontic intrusion of maxillary incisors and provisional composite restoration.
A. Pretreatment. B. Orthodontic Intrusion with equal movement of the gingival margins apically. C. Post treatment with placement of composite restortions.
Furthermore, unless the patient is susceptible to root resorption. (ie. has the genetic predisposition that causes root shortening during orthodontics) then significant root shortening will not occur regardless of the amount of tooth intrusion.10
For the Virtual Smile Design, the patient’s maxillary central incisors were intruded 3mm and proclined to the most ideal inclination. (Figs. 7,8). This provided an accurate estimate of what the patient could expect as a treatment goal. The improvement in dental esthetics and what amount of presurgical overjet would occur prior to orthognathic surgery.
Fig. 7

Treatment goal of maxillary (and mandibular) incisor position.
Fig. 8

Dental “decompensation” in preparation for orthognathic surgery.
A. Pretreatment. B. Pre surgical overjet preparation of 9mm. C. Post treatment.
Treatment Plan and Sequence:
Having determined the cause of the excessive deep overbite from the diagnostic assessment, a formalized treatment plan included the following:
Step 1. Full fixed orthodontic appliances to level the maxillary and mandibular arches and to position the maxillary central incisors in their most ideal position, taking into account the amount of over-eruption and wear.
This phase of treatment would reverse the dental compensations (“decompensate”) which have occurred due to the patient’s skeletal imbalance therby resulting in a temporary worsening of the facial profile and an increase in overjet in preparation for Step 2 (Fig. 8).
Step 2. Mandibular advancement via a bilateral sagittal split osteotomy (BSSO) with downward/clockwise rotation of the mandible. This will increase the anterior vertical dimension while maintaining the posterior vertical dimension by keeping the posterior contact between the maxillary and mandibular second molars (Fig. 9). This also improves the facial balance and musculoskeletal stability for the patient.
Fig. 9

Post treatment.
With this surgery, rigid internal fixation with small titanium screws is used to approximate the proximal and distal sections of the mandible. Rigid internal fixation is done in lieu of ‘wiring the jaws shut’ as so many clinicians still believe.
Step 3: Post-orthognathic surgery. Orthodontic finishing and provisional restoration to the worn maxillary and mandibular anterior teeth with composite bonding occurs six months prior to orthodontic bracket removal. The teeth that needed intrusion were retained in the intruded position to allow the collagen fibers to reorient themselves from an oblique position to one perpendicular to the tooth root and socket wall.10
Step 4: Retention for 6 to 9 months prior to definitive restorations to the maxillary central incisors only.
Treatment Outcome: (Figs. 9,10)
15 Years Post Treatment: The patient elected not to have his provisional composite restorations on the maxillary incisors replaced with composite or other restorative material. (Fig. 11).
Fig. 10

Improvement in facial proportions.
Fig. 11

Fifteen years post treatment.
Note: initial composite restorations on maxillary incisors and mandibular anterior teeth were never replaced.
Summary
The outcome would have been suboptimal , and more destructive to the existing dentition had an orthodontic option not been available to the patient.
The problem typically seen in patients with anterior tooth wear is that they experience compensatory eruption. Orthodontists have the ability to intrude these over-erupted incisors to achieve inter-occlusal space to allow for conservative restoration of these teeth. In essence, it allows for the replacement of the lost tooth structure. Orthodontic movement has the added benefit of aligning the gingival margins to an optimal position. A common misconception is that patients with anterior tooth wear are only “overclosed” with treatment aimed at increasing the vertical dimension through extensive posterior restorations. This ignores the fact that over-eruption of the anterior teeth has occurred and leads to an erroneous and more restoratively intense treatment plan.
Ideally, treatment planning for these types of cases should concentrate on whether incisor intrusion is possible along with a need to increase the vertical dimension through other means such as surgery. In doing so, the final restorative plan is typically less involved and more conservative.11
The appropriate treatment and sequencing is only possible by properly diagnosing the source of the problem.
Oral Health welcomes this original article.
References
- Kokich, Vincent G.: Altering Vertical Dimension in the Perio-Restorative Patient: The Orthodontic Possibilities in Interdisciplinary Treatment Planning ed. Michael Cohen. Quintessence Publishing 2008
- Magne, P., Galucci, G., Belser, U. Anatomic crown width/length ratios of unworn maxillary teeth in white subjects. J Prosth Dent Vol 89 No. 5, 453-461.
- Moss JP, Linny AD, Lowey MN. The use of three-dimensional techniques in facial esthetics. Semin Orthod 1995; 1: 94-104
- Andrews WA. AP relationship of the maxillary central incisors to the forehead in adult white females. Angle Ortho. July 2008. Vol 78, No.4. 662-669
- Coachman C., Calamita MA, Sesma M, Dynamic documentation of the smile and the 2D/3D digital design process. Int J of Perio and Rest Dent Vol 37 Issue 2 March/April 2017 pp 183-193
- Jafri, Z., Ahmad, N., Sawai, M., Sultan, N., & Bhardwaj, A. (2020). Digital Smile Design-An innovative tool in aesthetic dentistry. Journal of oral biology and craniofacial research, 10(2), 194–198
- Kokich, VG, Nappen, DL, Shapiro, PA, Gingival contour and clinical crown length:their effect on the esthetic appearance of maxillary anterior teeth. Am J Orthodont Vol 86 Issue 2, pp 89-94, 1984.
- Sarver, David M., The Importance Of Incisor Positioning in the Esthetic Smile: AJO-DO. Vol 20 Issue 2, pp 98-111. 2001
- Kokich,VG, Spear F., Kokich VO. Guidelines for treating the orthodontic-restorative patient. Semin Orthod 1997: 3:3-20
- Reitan, K. Clinical and histologic observations on tooth movement during and after orthodontic treatment Am J Orthodont 1967: 53: 721-725
- Magne, Pascal, Bonded Porcelain Restorations in the Anterior Dentition: A Biometric Approach, Quintessence Publishing, 1997.
About the Author
 Dr. Elliott is in the private practice of orthodontics in Prince George, British Columbia. He is a Clinical Assistant Professor in the Graduate Orthodontics Program at the University of British Columbia and a guest lecturer at the Graduate Orthodontics Program at Western University . He is also a Diplomate of the American Board of Orthodontics and is a Member of the Northwest Component of the Edward H. Angle Society where he serves on the Admissions Committee. Dr. Elliott is a proud member of Corus Orthodontists.
Dr. Elliott is in the private practice of orthodontics in Prince George, British Columbia. He is a Clinical Assistant Professor in the Graduate Orthodontics Program at the University of British Columbia and a guest lecturer at the Graduate Orthodontics Program at Western University . He is also a Diplomate of the American Board of Orthodontics and is a Member of the Northwest Component of the Edward H. Angle Society where he serves on the Admissions Committee. Dr. Elliott is a proud member of Corus Orthodontists.
RELATED ARTICLE: Principles of Smile Design Treatment Planning


