Continued Advancements in Full-Arch Implant Restorations
INTRODUCTION
Full-arch, implant-supported reconstruction continues to provide viable solutions to restore and improve function, enhance aesthetics, and change the quality of life for our patients. All-on-X implant reconstruction has benefitted from new advancements and technical innovations. In this current edition, the authors continue the journey, navigating through new developments that impact the full-arch analog and digital workflows. Our previous articles introduced several elements to aid the clinician in both the surgical and restorative phases of full-arch replacement, including the use of CBCT guided surgical applications1 and how they have greatly improved the assessment for implant placements relative to the desired restorative positions for preliminary and definitive restorations while also reducing implant complications. The authors have previously described an ancillary surgical protocol that utilizes extracted teeth as an autologous solution2 to bone grafting. This has greatly enhanced healing and long-term alveolar stability and provided ample graft volume while significantly reducing biomaterial costs. Subsequent publications also reported on improving the restorative time and treatment outcomes utilizing iJig technology3 and employing small-hole technology (C2F) to enhance the physical integrity and anatomy of milled or 3D printed provisional restorations4 and improving inter-arch alignment and occlusion. The goal of these articles has been to improve time, efficiency, costs, and long-term results for the betterment of clinicians, laboratory technicians, and patients. This latest article endeavors to provide updates in the acquisition of data necessary to complete the restorations with an emphasis on addressing improvements in screw-retained full arches for monolithic restorations that incorporate multi-unit abutments.
Data Acquisition
As the dental industry continues to strive for fully digital solutions, the development and improvement of intraoral data devices and acquisition technology has continued to evolve. Intraoral scanning (IOS) speeds and accuracies have become a viable solution for replacing direct analog impressions. Native IOS software applications now provide several impressive features that enhance and streamline complete digital protocols. However, due to inherent logistical limitations, the difficulty and accuracy of IOS technology used for full-arch dental implant restorations has presented major obstacles requiring additional applications to achieve fully digital solutions.
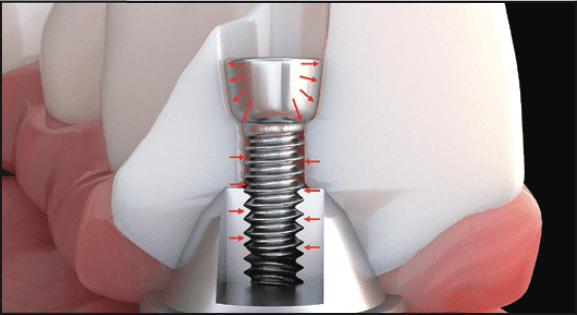
All-on-X, fixed surgical and restorative protocols require the placement of 4 or more implants with a favorable anterior-posterior spread to achieve the necessary long-term support. Capturing the positions of these implants with accurate cross-arch intraoral scanning, especially in the mandible, has been one of the major struggles for clinicians and dental laboratory technicians to overcome. IOS technology requires a stable environment for data to be stitched and captured accurately. Several techniques have emerged to aid the clinician in scanning these difficult environments, including proper retraction; salivary flow; lack of stable, keratinized soft tissues; large distances between scanning objects; and more. The use of splinting scan bodies with bands or wires (Figure 1) has facilitated the ability of scanners to continue a scan without interruption by creating a linear path for data capture.5 Innovative techniques, such as the sigma composite curve (or surgical intervention of fiducial markers fixated to the bone), have also helped improve scanning flow.6 While these processes work for some and not for others, developers have created alternative workflows to aid in acquiring accurate intraoral data.
Figure 1. Rubber bands, splinted wire frames, or applying composite directly to the tissue (Abelian sigma curve) aids intraoral scanners in acquiring accurate data.
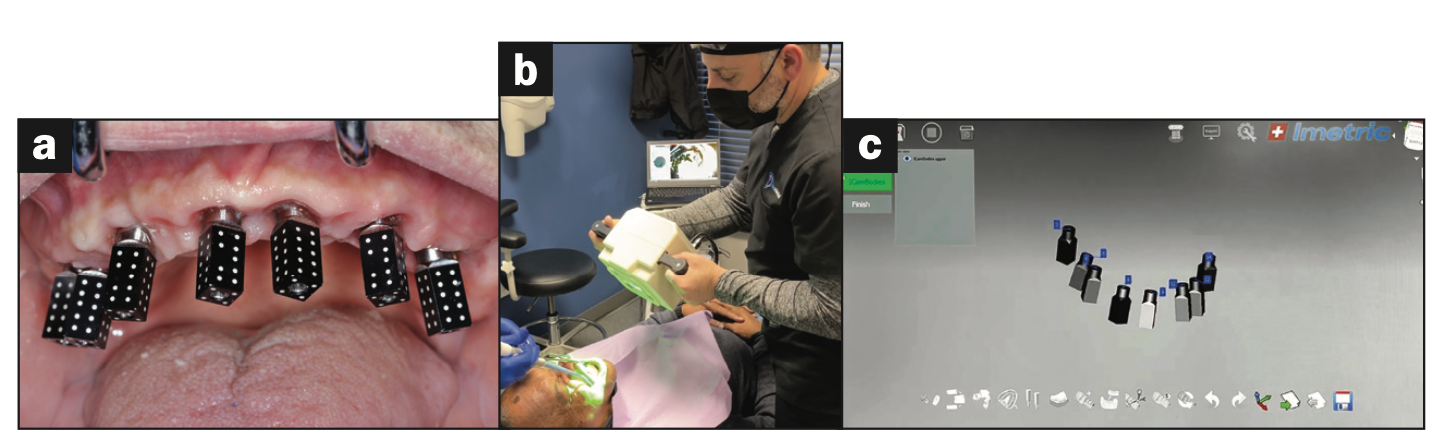
Figure 2. Photogrammetry (PG) uses an extraoral light source with manufacturer-specific scan abutments (iCam4D [Imetric]) to capture data for the PG software.
Photogrammetry (PG) in dentistry is a relatively new development that has revolutionized capture and positional analysis.7 PG is a diagnostic and research method using an extraoral capture device with specific photogrammetric scanning abutments to acquire measurements from 2D digital images (Figures 2a and 2b). PG scans allow dental clinicians to acquire precise measurements of individual scan bodies (Figure 2c) secured to dental implants as they are in their natural state8 either at the time of surgical placement or after the implants are uncovered. While extremely accurate for recording the spatial positioning of the implants, PG does not acquire the topography of the soft tissue. Therefore, a second scan is required with an intraoral scanner. The IOS data can then be used to fabricate a virtual 3D model used to measure various parameters of the implant analogs.9 The software correlation of these measurements can be used to assess and validate the correct positioning of implants and the alignment of a patient’s occlusion, size, distance, and angle. The combination of IOS and PG data provides the CAD software designer with all of the necessary information to virtually create a provisional prosthesis or a final restoration to be 3D printed or CAM-milled. The advanced capability of this highly accurate technology generates a fully digital workflow. There is little need for an analog model for production or verification purposes. While these impressive devices are extremely accurate, the initial purchase costs and availability of sensitive component materials have been an issue of concern.
To obviate the expense of PG, alternative fully digital workflows have been developed, such as the Abeniam XCell10 process, to facilitate and streamline data acquisitions, avoiding the need for PG. This proprietary workflow protocol requires education and the use of proprietary scan bodies. The XCell proven process is extremely efficient and paved the way for other intraoral technology to continue to be developed. To maintain consistency and accuracy, the protocol recommends a specific IOS device and CAM unit. Additionally, the workflow recommends the use of the “Abenaim powerball” screw to complete the production of the final restoration. While the recommendations are not mandatory, there is limited support when not utilizing the components as indicated within the protocols.

Figure 3. (a) Grammetry utilizes sophisticated scan bodies with extensions allowing splinting for increased accuracy and stability (OPTISPLINT [ROE Dental Laboratory]) and (b) shows the completed intraoral structure secured to an MUA with conventional screws.
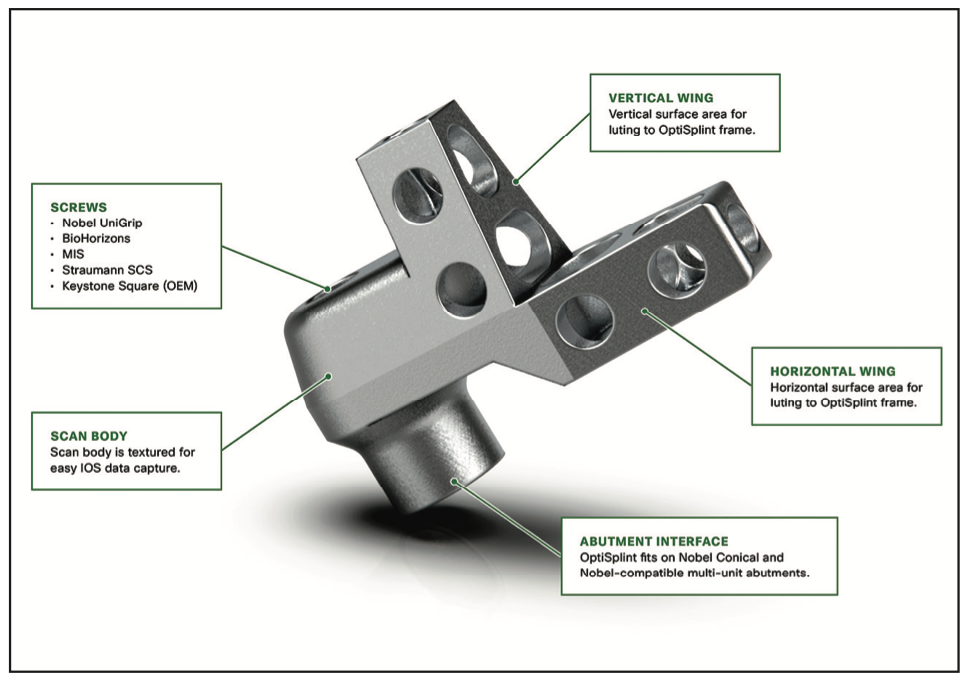
Figure 4. Grammetry scan body with vertical and horizontal extensions or wings to aid in bonding to resin mesh.

Figure 5. (a) Chrome osteotomy drill guide used for “full-template” guidance. (b) MUAs seated onto implants. (c) A provisional PMMA with holes to pick up the titanium cylinders. (d) A provisional restoration placed over grafting and platlet-rich fibrin after suturing. (e) At 4 months postoperative, remarkable soft-tissue healing was seen. (f) OPTISPLINT was luted intraorally and then scanned extraorally. (g) An iJig transitional restoration with analogs scanned extraorally. (h and i) FP1 restoration virtual exocad design. (j) The model was fabricated to test the fit of OPTISPLINT and final restorations. (k) The final monolithic metal-free zirconia restoration secured with Powerball screws. (l) Panoramic radiograph verifying the fit of the prosthesis, the direct seal, and that there were no gaps.
Another very recent workflow, termed Grammetry, has been developed as an open comprehensive surgical and restorative solution that offers a very similar and straightforward process with a significantly reduced cost and allows the use of existing IOS scanners. While PG requires the use of an expensive device and expensive scanning abutments, Grammetry requires the use of an existing IOS device along with special components provided to the clinician for each case. An analog-digital process utilizes MUA-compatible scan bodies (OPTISPLINT [Digital Arches]) designed to incorporate an aluminum mesh frame (Figure 3a) that can be customized chairside (with the included “snipping” tool) as required by the intraoral location of the implants. This mesh frame comes in small and large sizes to accommodate various mouth sizes and multi-unit abutment-implant positions. The workflow consists of inserting the scan bodies onto the MUAs intraorally (Figure 3b). The proprietary scan bodies have extensions (Figure 4) to allow the mesh to seat and rotate in close proximity, in turn, to allow luting using a resin base material (Stellar DC Acrylic [TAUB Products]). The structure can then be digitized by scanning intraorally with an IOS or extraorally with an IOS or a desktop scanner. The bonded splinting of the scan bodies to the mesh frame allows for a simple, uninterrupted scan path. The Grammetry process provides the clinician with the fully digital benefits of PG while also providing the capability to fabricate physical analog models that can be articulated as part of the prosthetic design process represented by the clinical workflow in Figure 5. Additionally, the Grammetry splint can be used as a model-verification jig. The fully digital Grammetry process communicates the necessary records workflow to design and fabricate a full-arch prosthetic at a significantly reduced cost to the dental laboratory. For those who have 3D printers and wish to design and print the provisional prosthesis, a calibration device is included in the Grammetry kit. This device will ensure that the specific printer settings based on the resin used will have a passive fit.
Ti-Base, or Not Ti-Base? That Is the Question
The desire for screw retention over fixed, cementable prostheses has been debated for some time.11 As restorative components have evolved and CAM software/hardware manufacturing capabilities have improved dramatically, screw retention utilizing multi-unit abutments has become the preferred choice for most full-arch restorations due to the passivity required with monolithic-zirconia-designed prostheses. The elimination of subgingival cement12 and the passivity of prosthetic seating can be attributed to the success of screw-retained, full-arch, cross-splinted restorations.
Screw-retained, fixed implant prosthetics have undergone many iterations over the past several decades.13 PMMA acrylic denture conversions proved too weak to withstand forces of occlusion long-term. In order to improve strength, metal-frame reinforcement was added to the acrylic. The end results still yielded a high level of long-term prosthetic failures. Improvements in ceramo-metal restorations yielded improved long-term aesthetics and longevity; however, the associated costs became a factor, and fractures continued to occur. With the strength and diversity of materials improving and CAD/CAM technology continuing to develop, other material choices have become more viable. Currently, monolithic zirconia has become the most widely used material for full-arch, implant-supported restorations.14,15 The milled and sintered zirconia structure could be fabricated with a standard multi-unit abutment coping, custom-milled titanium bar, or a Ti-base cap. These metal substructures are chemically luted to the zirconia structure (Figure 6). Fractures were still evident, most notably from poor design. The fractures tended to occur in distal extensions attributed to poor A-P spread and in locations of screw-access holes. Screw-access fractures could be contributed to the lack of zirconia thickness in the crown-abutment interface. Conventional prosthesis-retaining screws secured to the MUAs have a screwhead that is 2 mm in diameter, only allowing for 0.25 mm of screw surface to engage the crown portion (Figure 7). This leaves only 0.4 mm between the head of a conventional screw and the titanium base. Reports of screw loosening, screw fractures, and de-bonding of Ti-bases from the zirconia structure have become a source of difficulty and concern.16 Developers have searched for alternative solutions as these complications and avoidable remakes continue to persist.
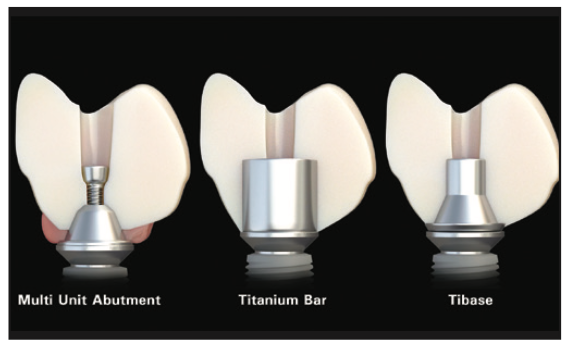
Figure 6. Three methods of attaching zirconia restorations to implants are illustrated here: via conventional MUA, Ti-bar, or Ti-base.
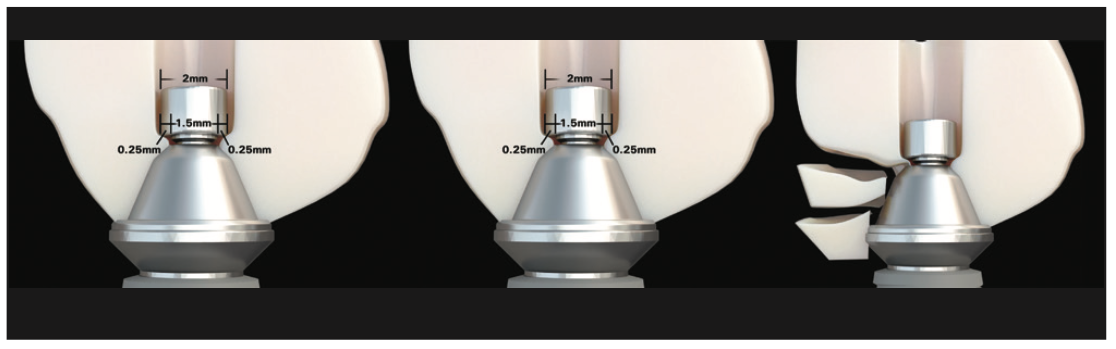
Figure 7. The dimensions of standard MUA screwheads and available zirconia, which can lead to fracture.
To counter the effects of screw-loosening, Ti-base de-bonding, and screw-access-hole fracture, several screws have been developed. Over the past few years, the continued refinement of these screws has led to the evolution of metal-free, full-arch monolithic zirconia restorations. As a result, in many case presentations, the need for excessive bone reduction to accommodate the metallic portion has been eliminated, allowing for increased potential for FP1 vs FP3 restorations. Some of these screws allow for increased thickness of zirconia between the MUA and screwhead. Allowing increased thickness in this susceptible region further reduces the risks of zirconia fracture in the screw-access-hole location. Additionally, the design of the newer screws typically has a tapered or rounded screwhead, allowing for improved retention by applying pressure to the lateral walls in the apical direction, reducing incidences of screw loosening.
A few of these newer screw designs can accommodate “angled” screw channels. Angled screw channel correction has become widely incorporated in single-tooth implant restorations.17 Previously, correcting angulations for full-arch restorations on multi-unit abutments required using an MUA with an increased degree of angulation. When an MUA is secured to the implant and the scan data has been captured, altering the screw-access channel would then affect the angulation of the MUA, which would need to be replaced. This becomes problematic when provisional or final restorations have already been designed and a new desired positional tooth change is requested. Often, these changes can leave access holes in aesthetic or potentially vulnerable areas (Figure 8). Additionally, there are angular limitations of the MUAs, which vary with each component manufacturer. Rather than changing the MUA and dealing with the difficulties of temporization, some of the newer MUA screw technologies allow for the MUA to remain in place while the screw channel can be angulated as much as 25°. One screw in particular that is uniquely designed is the “La Vis Grammetry” screw (Figure 9). The La Vis screw can accommodate various vertical positional depths. This feature allows for accommodating directly to an MUA, Ti-base, or Ti-bar simply by adjusting the height position of the screw. The adjustable vertical position allows for more or less zirconia, if desired, depending on available interocclusal space. In addition to accommodating angled screw channels, the ideal screw-access position and depth can be achieved.
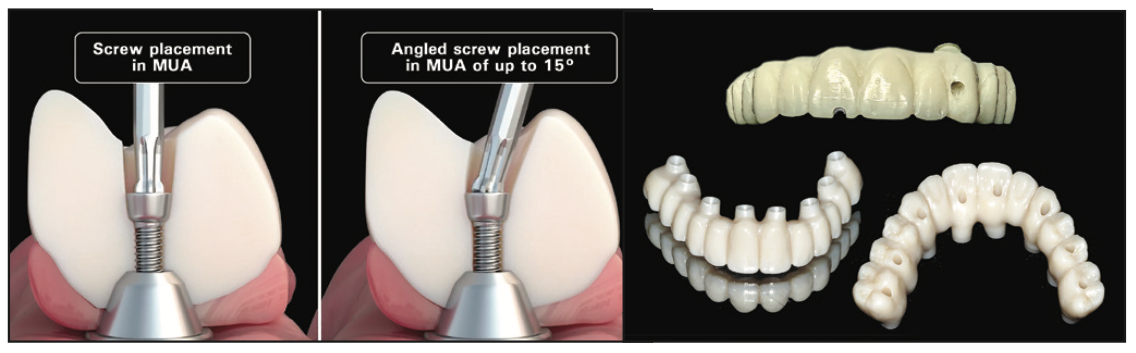
Figure 8. (a) Illustration of angled vs straight screw channels and variation in access hole positions for improved strength and aesthet- ics. (b) Using an angled screw channel can result in up to a 25° change in angulation.
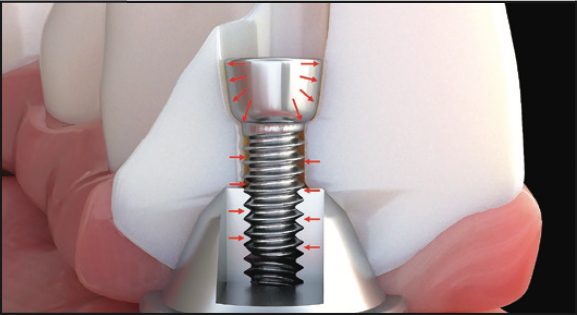
Figure 9. La Vis Grammetry screw direct-to-MUA allows for an increased thickness of zirconia dependent on available interocclusal space. (Image courtesy of Dr. Danny Domingue.)
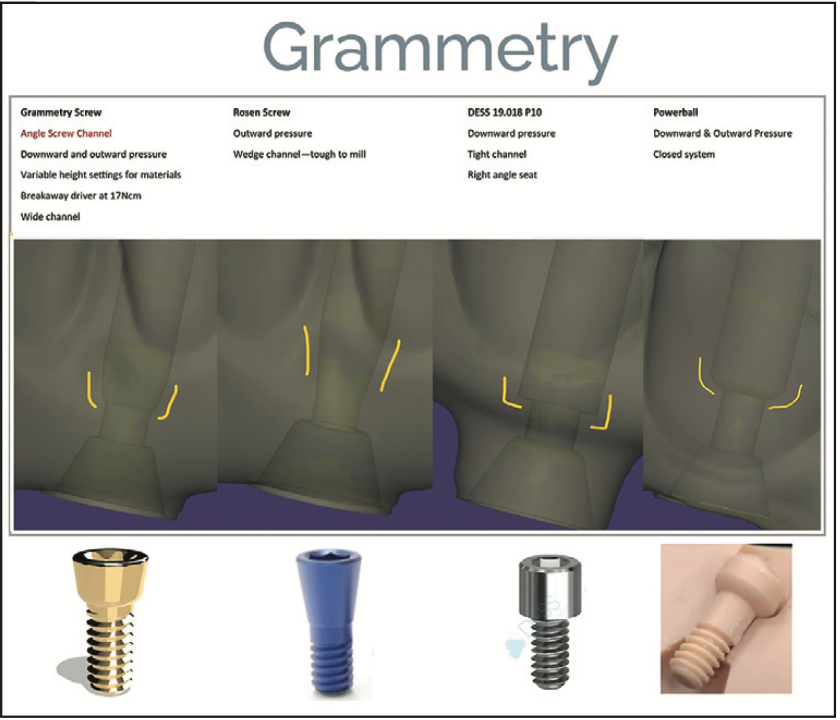
Figure 10. New and innovative screw technol- ogy features and benefits with design and torque information.
Therefore, by utilizing the innovative methods of data capture and validation, combined with newer screw technology, it is possible to accomplish increased efficiency and accuracy of the fabrication process. Additionally, it has been illustrated that screws that can accommodate an angled screw-access channel position will result in improved aesthetics. The benefits of these screws and driver are required for usage (Figure 10).
CASE REPORT
The following case exhibits the features and benefits of utilizing Grammetry in combination with innovative screw technology. A 63-year-old male patient with non-contributory medical history presented with failing dentition in both arches. The mandible contained an impacted canine as well as several mobile and painful teeth (Figure 11a). The maxilla was in similar condition with deteriorating, painfully mobile teeth, as well as extensive caries. While the bone loss was significant in the mandible, the vertical dimension allowed for both arches to be treated with an FP1 (fixed prosthetic 1 Misch classification18) manor.
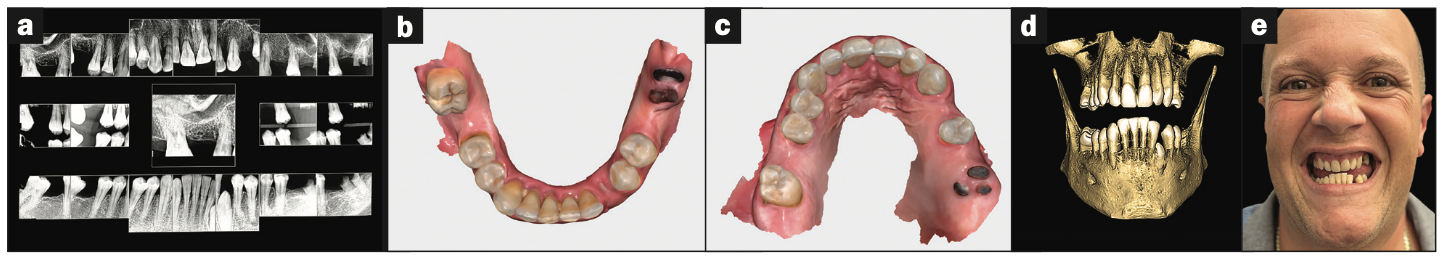
Figure 11. (a) Full-mouth x-ray series revealing decay and periodontal defects. (b and c) Upper and lower IOS scans (Medit). (d) CBCT for diagnosis and treatment planning (Carestream Dental). (e) Preoperative photo showing the reverse-curve of the lower teeth and poor aesthetics.
Diagnostic records were collected, including intraoral digital impressions (i700w [Medit]) (Figures 11b and 11c), large FOV 3D CBCT imaging (CS 9600 [Carestream Dental]), full-mouth digital x-rays (Figure 11d) (RVG 6200 [Carestream Dental]), and intraoral and extraoral photographs (Figure 11e). Based on the assessment of the acquired data, several treatment plans were developed and presented to the patient. Conventional treatment concepts that were considered included salvaging those teeth deemed stable enough to be utilized to retain removable appliances, implant stabilization with a combination of fixed and removable prosthetics, implant-supported overdentures, and full-mouth reconstruction with implant therapy. After reviewing the various treatment proposals, the patient elected for full-arch, fixed replacement with implants. The collected data along with preliminary plans for potential implant receptor sites (Blue Sky Plan [BlueSkyBio]) were submitted to the laboratory (ROE Dental Laboratory) for review. The 3D data from the CBCT scan was then merged with the IOS data set to aid in determining a restoratively driven solution for both arches. The laboratory then designed transitional full-arch, screw-retained restorations utilizing CAD software at the designated vertical dimension required for the prostheses. The desired tooth position, as visualized with the 3D reconstructed volume of bone, helped to determine the most favorable implant receptor sites. A virtual remote planning session was held with the laboratory to finalize the “full-template” guided surgical plan (CHROME GuidedSMILE), which incorporated a 2-mm increase in VDO, and it was sent for production. The CHROME GuidedSMILE protocol consists of several component parts that provide a “stackable” solution with metallic scaffolding to control the bone reduction; the preparation of the osteotomies; full-template guidance of the implants into the bone; implant depth, trajectory, and rotational indexing; the positioning of the MUAs; and the delivery of the provisional restorations.1

Figure 12. Using extracted teeth to achieve autologous bone volume using the Smart Dentin Grinder (KometaBio).
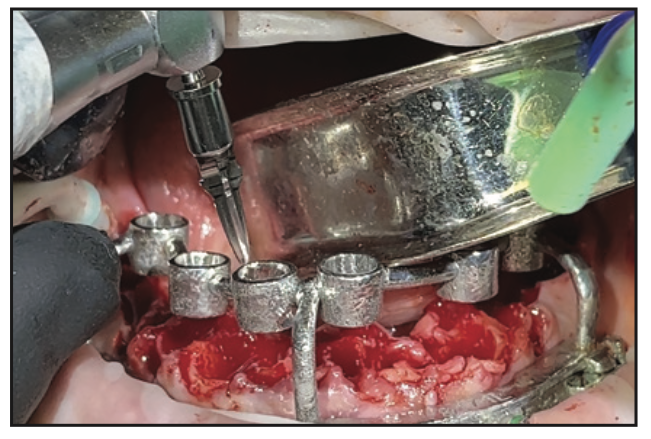
Figure 13. Universal Shaper drills (ROE Dental Laboratory) were used for guided osteotomy preparation with CHROME GuidedSmile.
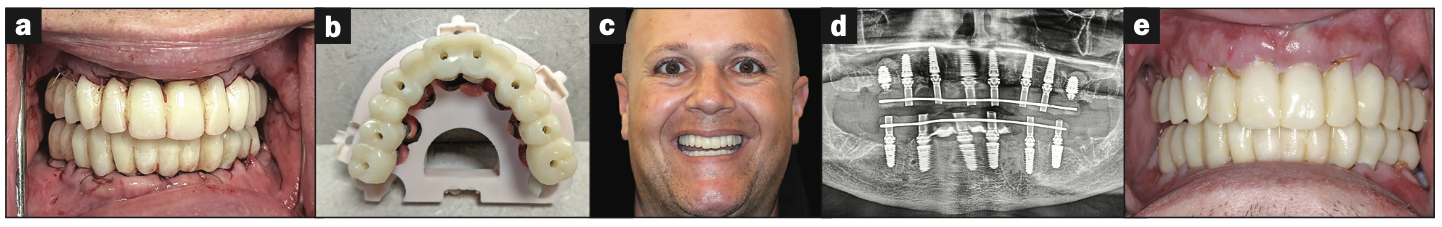
Figure 14 (a) Retracted view of transitional restorations fabricated with (b) C2F small-hole technology. (c) Two-week post-op smile. (d and e) The panoramic radiograph and intraoral photos revealed excellent healing.
The entire maxillary and mandibular arch surgery was completed in a single visit under IV sedation. All remaining teeth were extracted, and selected teeth were then pulverized utilizing the Smart Dentin Grinder (KometaBio) and sterilized for autografting bone substitute2 (Figure 12). A biologically driven drilling system for anatomic alveolar sculpting (Universal Shapers [ROE Dental Laboratory]) was employed (Figure 13). The alveolar bone was scalloped utilizing the diamond shaper drills for both implant and pontic sites to promote emergence profiles for enhanced aesthetics following the basic tooth size requirements assessed from the initial data collection. The surgery was uneventful except for a mild complication during the removal of the impacted lower canine. Implant stability was measured with resonance frequency analysis (ISQ) to validate loading protocols. MUAs were secured to each implant based on the rotational positions as predetermined by the surgical planning. Deficient sites and residual tooth sockets were then grafted with dentin ground autograft, covered with platelet-rich fibrin membranes, and sutured around healing abutments. Provisional restorations were fabricated using the C2F protocol4 (Figures 14a and 14b). After customizing and polishing the provisionals, the restorations were inserted and allowed to heal (Figure 14c). A postsurgical panoramic radiograph illustrating maxillary and mandibular implants with transitional restorations in place was taken (Figure 14d). A 2-week retracted view of transitional restorations can be seen in Figure 14e.
During the subsequent postoperative visits, the patient described being extremely happy with his newly rehabilitated mouth. As the preliminary provisional restorations were designed based on a desired virtual result, it was possible to make changes as necessary for the final restoration. A slight discrepancy was observed in initial tooth size and midline position, which were noted to be corrected during the finalization of the monolithic zirconia restoration. The patient tolerated the 2-mm increase in VDO with minimal adjustments to occlusion accomplished through digital articulation (Occlusense [Bausch GmbH & Co KG]). Tissue healing was unremarkable except for a minor loss in alveolar height and soft tissue from the impacted canine removal site. After 4 months, the patient returned to complete the process of finalizing the definitive prosthesis. Final records were taken, including new digital scans and photos. Photos included patient profiles with and without a smile as well as intraoral occlusion. The digital scans included a facial scan acquired from the CBCT device (CS 9600), an upper and lower soft-tissue scan (i700w) using scan bodies (Dess), bite registrations, an iJig scan of the provisionals for tooth positions,3 and PG (ICam4D [Imetric]) and Grammetry scans (Figure 15). The Grammetry scans were scanned extraorally with both an intraoral scanner (i700w) and extraoral desktop scanner (T710 [Medit]) for comparison.
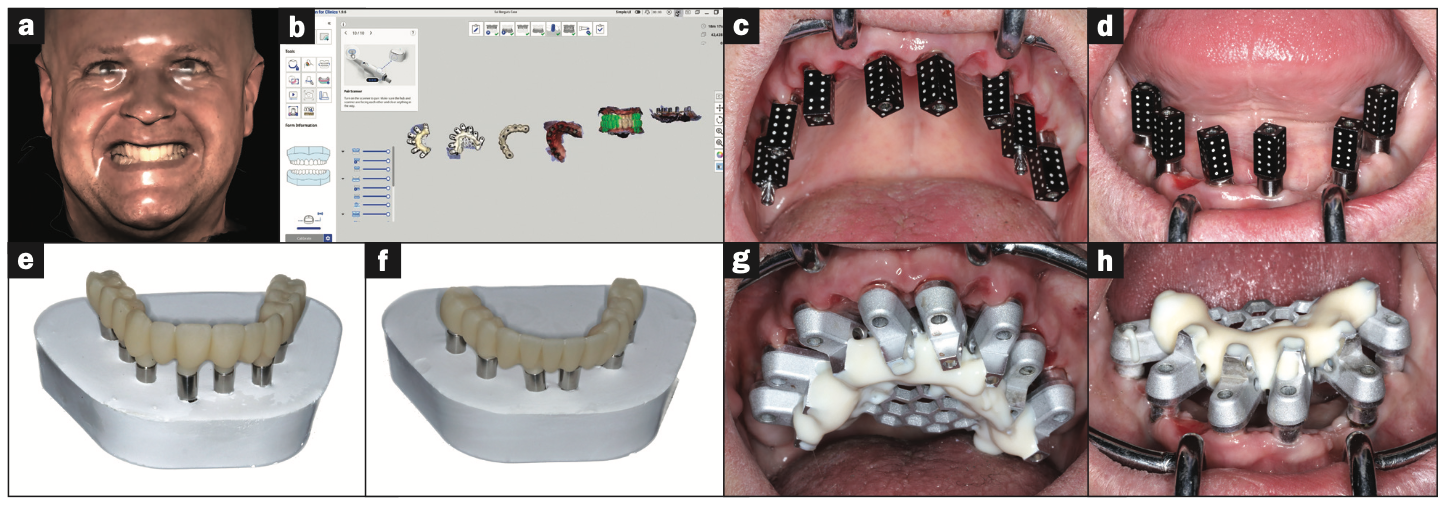
Figure 15. (a) Facial scan for smile evaluation and midline assessment. (b) IOS Grammetry workflow for transfer to the dental labora- tory (Medit). (c and d) PG scan abutments were used to validate and confirm Grammetry implant positions (Imetric). (e and f) Three- dimensional printed upper and lower restorations on verification casts. (g and h) Grammetry OPTISPLINT was used to capture implant positions for model fabrication.
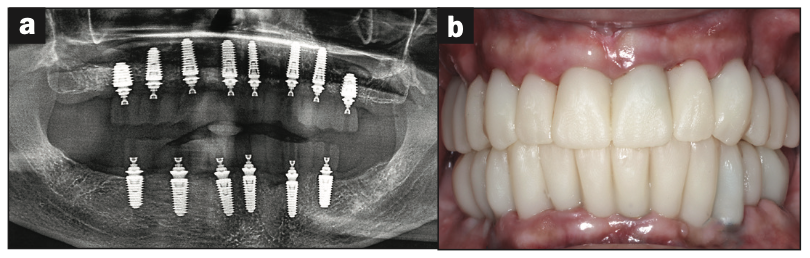
Figure 16. (a) Panoramic radiograph showing printed restorations secured with La Vis Grammetry screws. (b) The retracted, intraoral view.
The data collected was sent through the scanning software portal (“Medit scan for Clinics”) to the dental laboratory (ROE Dental Laboratory) with the requested changes to correct the desired smile design. Utilizing advanced planning features in the design software (exocad), the midline and tooth-size changes were corrected. Upper and lower 3D printed PMMAs were used for try-in using the direct-to-MUA screws (Le Vis Grammetry) (Figure 16a). Fit, phonetics, aesthetics, and occlusion were evaluated and confirmed using digital articulation (Occlusense) (Figure 16b). The patient was extremely satisfied with the printed try-in. Since no adjustments were required, the patient was allowed to leave with the printed try-in as new provisionals made from extra-strong resin. The new provisionals were utilized for 10 days to confirm form and function. The final shade was chosen, and the laboratory fabricated metal-free monolithic zirconia restorations.
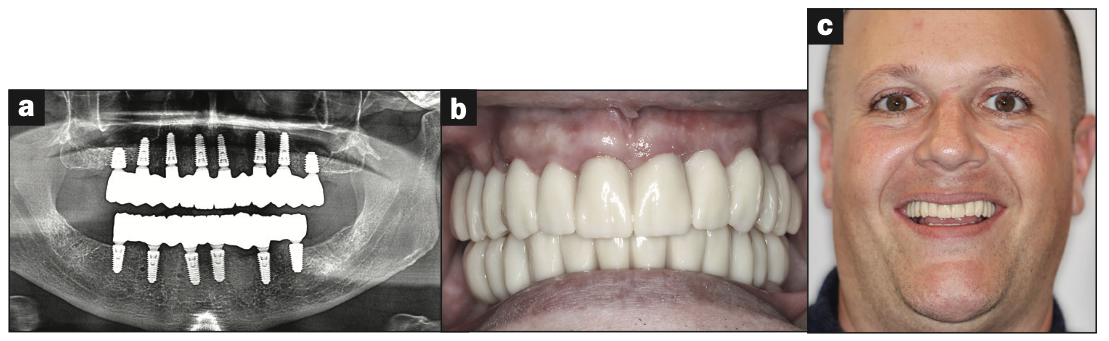
Figure 17. (a) Final panoramic radiograph confirming seating of monolithic zirconia restorations. (b) The intraoral, retracted view. (c) The final patient smile, showing excellent aesthetics and a happy patient.
Final restorations were passively, accurately, and uneventfully seated 10 days later using Grammetry screws (Le Vis). Confirmation records, including fit, function, phonetics, and occlusion, were all rechecked and confirmed with photos, radiographs, and digital articulation (Figure 17a). The patient was extremely satisfied with his final restorations, describing the process as “life-changing” and surprisingly fast compared to what he had heard about full-mouth implant therapy. He was especially pleased with the speed at which the final process was able to be completed (Figures 17b and 17c).
CONCLUSION
Full-mouth single or dual-arch implant reconstruction can be completed in a timely manner under ideal circumstances with a foundation of proper diagnosis and treatment planning. The implementation of restoratively driven guided surgery can improve accuracy and ensure proper implant placement, depth, and angulation. Data collection at either the time of surgery or post-op can improve the accuracy and speed at which finalization can be completed.
The present case described digital and analog protocols for capturing soft-tissue topography as well the use of iJig provisionals essential to aligning and validating the intraoral position of restorations, additionally with Grammetry and PG. Voids can be accurately shown and adjusted to be filled in using design software. With the incorporation of a 2D profile photograph or, better yet, a 3D facial scan, tooth position, size, and shape can be easily managed for an improved try-in or final restoration.
In this case, 3 methods were utilized to capture data to provide a basis for comparison. The first is PG, which has been acknowledged as the gold standard for implant-position accuracy. The second is Grammetry, which utilized the new OPTISPLINT analog luting protocols. The third is digital capture utilizing the OPTISPLINT Grammetry, in which the intraoral scanner and extraoral desktop captures were analyzed and compared. The extraoral desktop capture of the OPTISPLINT Grammetry was almost identical to the PG capture when both data sets were superimposed. The extraoral desktop capture of the Grammetry splint yielded marginally better results than the intraoral scan captured extraorally. While results may be slightly less accurate due to the human error associated with intraoral scanners, they were more than acceptable, as CAD/CAM unit tolerances cannot mill beyond the obtained results. The added benefits of using the Grammetry process enable a physical model to be produced, allowing for physical mode production for an analog try-in for both printed try-in and final milled restorations.
In summation, there are various existing digital workflows that can be successfully utilized to achieve consistent and accurate results for full-arch, implant-supported restorations. Currently, due to supply-chain shortages and limitations, PG devices are back-ordered and in short supply. Grammetry protocol components are less expensive and available. For the purposes of this case presentation, it was found that the analog/digital protocol of Grammetry can be used as an effective, affordable, and equally accurate alternative to PG. In combination with other necessary records, Grammetry can provide a fully digital capture of implant positions while providing analog models, if desired, for articulation and restorative fabrication. Capturing data either on the day of surgery or later can greatly improve dental laboratory communication and reduce final prosthetic production time with a high level of accuracy, enhancing the overall clinical and patient experience. Future research on the protocols and materials utilized for this case presentation is recommended as the search for the most economical and accurate digital workflows continues to evolve.
REFERENCES
1. Ganz SD, Tawil I. Full-arch implant surgical and restorative considerations: utilizing a full template guidance technique. Dent Today. 2019;38(9):72–8.
2. Ganz SD, Tawil I. Autologous tooth structure as an adjunct grafting modality. Dent Today. 2021.
3. Ganz SD, Tawil I. Full-arch implant surgical and restorative considerations: innovative digital workflow using a verification jig with teeth. Dent Today. 2020;39(1):70–6 .
4. Ganz SD, Tawil I. Continued innovation for full-arch immediate loading: small access hole technology. Dent Today. 2021.
5. Kim JE, Amelya A, Shin Y, et al. Accuracy of intraoral digital impressions using an artificial landmark. J Prosthet Dent. 2017;117(6):755–61. doi:10.1016/j.prosdent.2016.09.016
6. Papaspyridakos P, Chen YW, Gonzalez-Gusmao I, et al. Complete digital workflow in prosthesis prototype fabrication for complete-arch implant rehabilitation: a technique. J Prosthet Dent. 2019;122(3):189–92. doi:10.1016/j.prosdent.2019.02.004
7. Peñarrocha-Oltra D, Agustín-Panadero R, Bagán L, et al. Impression of multiple implants using photogrammetry: description of technique and case presentation. Med Oral Patol Oral Cir Bucal. 2014;19(4):e366-71. doi:10.4317/medoral.19365
8. Sánchez-Monescillo A, Sánchez-Turrión A, Vellon-Domarco E, et al. Photogrammetry impression technique: a case history report. Int J Prosthodont. 2016;29(1):71–3. doi:10.11607/ijp.4287
9. Azevedo L, Molinero-Mourelle P, Antonaya-Martín JL, et al. Photogrammetry technique for the 3D digital impression of multiple dental implants. In: Tavares J, Natal Jorge R. (eds) VipIMAGE 2019. Lecture Notes in Computational Vision and Biomechanics. Springer, Cham. 2019: 615–9.
10. Smile Syllabus. XCell dental implants. https://smilesyllabus.com/xcell-dental-implant-process-parts/
11. Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009;80(9):1388–92. doi:10.1902/jop.2009.090115
12. Tawil I. Avoiding peri-implantitis: key factors for improved clinical outcomes. J Oral Health. 2016.
13. Delucchi F, De Giovanni E, Pesce P, et al. Framework materials for full-arch implant-supported rehabilitations: a systematic review of clinical studies. Materials (Basel). 2021;14(12):3251. doi:10.3390/ma14123251
14. Larsson C, Vult Von Steyern P. Implant-supported full-arch zirconia-based mandibular fixed dental prostheses. Eight-year results from a clinical pilot study. Acta Odontol Scand. 2013;71(5):1118–22. doi:10.3109/00016357.2012.749518
15. Abdulmajeed AA, Lim KG, Närhi TO, et al. Complete-arch implant-supported monolithic zirconia fixed dental prostheses: a systematic review. J Prosthet Dent. 2016;115(6):672–7.e1. doi:10.1016/j.prosdent.2015.08.025
16. Gonzalez J, Triplett RG. Complications and clinical considerations of the implant-retained zirconia complete-arch prosthesis with various opposing dentitions. Int J Oral Maxillofac Implants. 2017;32(4):864–9. doi:10.11607/jomi.5369
17. Rasaie V, Abduo J, Falahchai M. Clinical and laboratory outcomes of angled screw channel implant prostheses: a systematic review. Eur J Dent. 2022;16(3):488–99. doi:10.1055/s-0041-1740298
18. Misch CE. Bone classification, training keys to implant success. Dent Today. 1989;8(4):39-44.
ABOUT THE AUTHORS
Dr. Tawil received his DDS degree from the New York University College of Dentistry and his Master of Biological Sciences degree from Long Island University. He is co-director of Advanced Implant Education. He is a Diplomate of the International Academy of Dental Implantology as well as a Fellow of the International Congress of Oral Implantologists (ICOI) and the Advanced Dental Implant Academy. He has received recognition for outstanding achievement in dental implants from the Advanced Dental Implant Academy and has received the President’s Service Award for his volunteer work. Dr. Tawil lectures internationally on advanced dental implant procedures. He maintains a general private practice in Brooklyn, NY, where he focuses on implant therapy. He can be reached at tawildental@gmail.com.
Dr. Ganz received his specialty certificate in maxillofacial prosthetics/prosthodontics. He is a Diplomate and Fellow of the Academy of Osseointegration, a Fellow of the International College of Dentists, US Ambassador of the Digital Dental Society, and co-Director of AIE. Dr. Ganz was recently honored by the American Academy of Implant Dentistry and the Digital Dental Society for his lifelong contributions. Dr. Ganz maintains a private practice in Fort Lee, NJ and Manhattan, NY. He can be reached at drganz@drganz.com.
Disclosure: The authors report no disclosures.