Subjects
Medical records and CBCT images of patients who visited the Department of Oral Medicine at Jeonbuk National University Dental Hospital between 2018 and 2020 with complaints of TMJ discomfort were reviewed.
Inclusion criteria were: (1) patients who underwent at least two CBCT scans of their TMJ by the same equipment, including their first visit; (2) patients who had been treated using conventional modalities including physical therapy, occlusal stabilization appliance (2 mm thick hard acrylic resin in the molar area; OSA), and medication; and (3) cases with consensus of the two experienced radiologists in the interpretation of the images. Exclusion criteria were as follows: (1) patients with other TMJ diseases such as condyle fracture, osteochondroma, osteomyelitis, rheumatoid arthritis, and systemic disorders affecting bone metabolism; (2) patients with facial trauma including TMJ; and (3) cases with blurry or poor CBCT images.
This study adhered to the Declaration of Helsinki. It was approved by the Institutional Review Board of the Jeonbuk National University Hospital (No. CUH2022-01–041). Informed consent was waived by the ethics committee (Institutional Review Board of the Jeonbuk National University Hospital) because of the retrospective nature of this study and the analysis using anonymous clinical data.
Clinical information
Clinical variables were collected from patients’ medical records. Clinical information recorded at the first visit of each patient, including the presence and degree of TMJ pain, limited ability to open the mouth (MOL), loss of posterior teeth, occlusal changes, and clenching habits were reviewed. The degree of TMJ pain was evaluated using a numerical rating scale (NRS). MOL was defined as the case where the maximum mouth opening range was ≤ 40 mm. Follow-up CBCT was performed after clinical improvement in pain and TMJ function. The duration of pain during the subsequent treatment process and decision to use an oral appliance were also considered. The time interval between the two CBCT scans was recorded. Demographic information associated with each participant is presented in Table 1.
CBCT scan
All CBCT scans were performed using an Alphard 3030 (Asahi Roentgen Ind., Co. Ltd., Kyoto, Japan) scanner with the following parameters: tube voltage, 80 kVp; tube current, 8 mA; FOV (field of view), 154 × 154 mm; and voxel size, 0.3 mm. Obtained images were reconstructed using the Ondemand3D software (CyberMed Inc., Seoul, Korea) for further analysis. Two TMJ scans, including those obtained during the first visit for each patient, were used to observe volume changes of the mandibular condyle in the same patient over time.
Radiological diagnosis
Two oral and maxillofacial radiologists diagnosed TMJ CBCT images for surface erosion, subcortical cyst, or osteophyte formation according to the TMJ CT criteria presented by the DC/TMD. Subcortical cyst was defined as a cavity below the articular surface that deviated from normal marrow pattern Surface erosion was defined loss of continuity of articular cortex. Osteophyte formation was defined as marginal hypertrophy with sclerotic borders and exophytic angular formation of osseous tissue arising from the surface.25 Image diagnosis was confirmed by two experienced radiologists with a consensus.
Image analysis
Image processing
The open-source software 3D Slicer (v4.11, Slicer, http://www.slicer.org/) was used for volumetric analysis of a total of 132 CBCT images of condyles of 66 subjects26. Image processing steps are shown in Fig. 2.
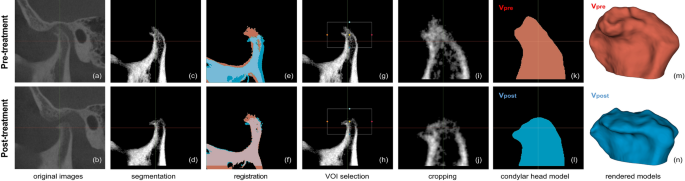
Image processing steps. (a–b) Original cone-beam computed tomography (CBCT) images of pre- and post-treatment from the same patient. (c–d) Pre- and post-treatment CBCT images after removal of cranial parts. (e–f) Alignment of pre- and post-treatment images by voxel-based registration and segmentation. Red segment, pre-treatment; Blue segment, post-treatment. (g–h) Selection of a common volume of interest (VOI) for both mandibles. (i–j) Cropped condylar head images by the common VOI. (k–l) Resultant segments of pre- and post-treatment condylar heads. (m–n) 3D model of each segment. Red, pre-treatment (Vpre); Blue, post-treatment (Vpost). The images were generated using the open-source software 3D Slicer (v4.11, Slicer, http://www.slicer.org/).
Segmentation
Using automatic threshold function with maximum entropy method in the segment editor module, bony parts from pre-treatment CBCT were segmented. The obtained threshold value was saved for the segmentation of post-treatment TMJ CBCT of the same patient. CBCT of TMJ usually included cranial parts (such as the glenoid fossa and zygomatic arch) and mandibular parts (such as the mandibular condyle, mandibular ramus, and coronoid process). Among the segments, only the mandibular part was selected while others were removed. When segmenting the mandible from post-treatment TMJ CBCT images, we used the threshold value obtained from auto-thresholding pre-treatment CBCT of the same joint. Using these mandibular segments as a mask, only voxels corresponding to the mandible were cropped from the original CBCT. Median filter with radius of two voxels was applied to these cropped volumes to minimize noise.
Registration and cropping
To measure volume change after treatment, pre- and post-treatment mandibles were aligned at the same location using a voxel-based automatic registration function in the registration module. With two mandibles superimposed, a common volume of interest (VOI) containing only the condylar head part was set. Using this common VOI, each mandibular head part was cropped to obtain aligned condylar heads. These cropped condylar heads were used in the volumetric analysis described below.
To check accuracy of segmentation and registration, an additional VOI containing the condylar neck and mandibular ramus was set directly below the VOI of the condylar head. This was used on the premise that while the volume of condylar head changes as DJD progressed, other areas of the mandible showed little changes. Using additional VOIs, regions containing the condylar neck and mandibular ramus were also cropped and used for volumetric analysis along with the condylar head. The more accurate the segmentation and registration, the smaller this volume difference would appear.
Assessment of condyle volume change
Using the threshold value applied in the previous step, two cropped condylar heads were re-segmented to generate segment masks. Using the model maker function, surface models of masks were created and volumes of models were measured from each model information. Volumes of pre- and post-treatment condylar heads were designated as Vpre and Vpost, respectively. The value obtained by subtracting the Vpre from Vpost was named as dV, indicating total volume difference after treatment.
To analyze detailed volume changes, net increase and net decrease of condylar volume were investigated. The volume obtained by subtracting the overlapping area from post-treatment segment was interpreted as a net increase (dV +) and the volume obtained by subtracting the overlapping area from pre-treatment segment was interpreted as a net decrease (dV− ). Names and interpretations of variables used in volumetric analysis are shown in Table 6 and a visualized example of this analysis is demonstrated in Fig. 3. Volume changes (dV, dV− and dV) underwent further analysis as shown below.
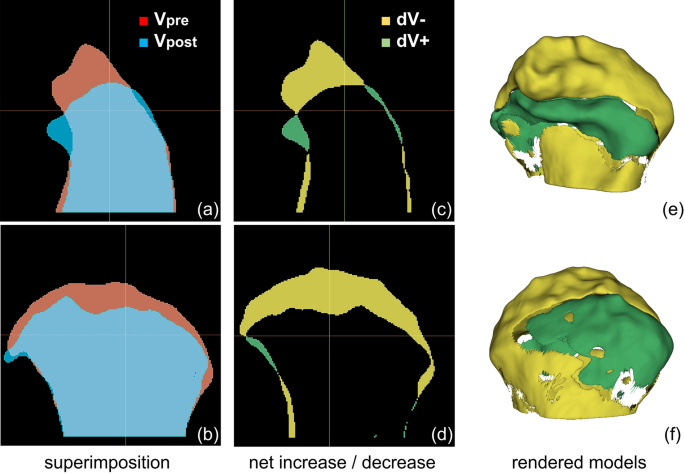
Representative volumetric analysis of processed cone-beam computed tomography (CBCT) images. (a–b) Superimposition of Vpre and Vpost in sagittal and coronal view. (c–d) Sagittal and coronal views of net decrease (dV− ) and net decrease (dV +). Yellow segment, dV− = Vpre− overlap; Green segment, dV + = Vpost-overlap. (e–f) Anterior and posterior views of the 3D model of dV− and dV + . The images were generated using the open-source software 3D Slicer (v4.11, Slicer, http://www.slicer.org/).
Data analysis
A total of 132 CBCT images of TMJ from 66 patients were included in this study. We analyzed differences in condyle volume changes (dV, dV− , dV +) between TMJs with and without surface erosion. Next, to investigate whether joint pain affected condyle volume changes when erosion was present, we compared condyle volume changes (dV, dV− , dV +) based on the presence or absence of TMJ pain using only 90 TMJ images with confirmed erosion.
We also investigated whether clinical factors influenced volume parameters. Cases with bilateral joint pain and surface erosion were excluded from this analysis because clinical factors were dependent on the patient, not the TMJ. We compared differences in volume parameters in 45 TMJ images based on the presence of various clinical factors.
Statistical analysis
Mann–Whitney U and Kruskal–Wallis tests were used to assess effects of clinical and radiological factors on condylar volume change because some experimental groups did not satisfy normality in Shapiro-Wilks test. Spearman’s correlation analysis and multiple linear regression analysis were used to determine relationships between variables. Statistical significance was set at p < 0.05.

