INTRODUCTION
Three-dimensional printing in dentistry has seen accelerating growth over the past several years with emerging applications in definitive restorations. Not only is the technology becoming increasingly cost-effective and user-friendly, but novel photopolymer resins are beginning to rival conventional materials in their durability and aesthetics, with some printed materials exceeding the mechanical properties of milled ceramics and hybrid ceramics.1,2
Printed restorations are a progressive solution to perform conservative indirect quadrant dentistry using inlays and onlays in a single visit. Partial-coverage restorations enable conservation of the remaining tooth structure, providing greater durability of restorations compared to full-coverage crown preparations that potentially unnecessarily remove healthy tooth structure.3-5 Many dental practices, however, avoid inlay/onlay restorations due to various challenges associated with both indirect and direct restorations. Typical indirect workflows require multiple office visits, including direct composite temporization while the restoration is being fabricated at a dental lab. While indirect restorations allow the use of more durable restorative materials, direct workflows are typically preferred due to fewer necessary office visits. As for direct composite restorations, many clinicians view them as requiring a more meticulous technique compared to the alternative of full-coverage crowns. With direct composite restorations, anatomical contacts and contours must be precisely hand-sculpted into the material. This can be particularly challenging with larger restorations when more material is removed during tooth preparation. Additionally, as the geometry of a tooth preparation increases in complexity, the failure rate with direct composite increases by 30% to 40% for every additional surface added to the restoration.6 A recent systematic review and meta-analysis showed that indirect onlay restorations made of resin were equally durable to ceramic restorations. Both performed dramatically better compared to direct resin restorations.7
Direct resins have 2 major drawbacks related to their polymer chemistry. First, due to their cross-linking mechanism, direct resins typically have a bond conversion ratio for their methacrylate esters of roughly 60%, meaning they are never fully cured.8 Several factors are involved in this low level of methacrylate bond conversion, including curing time, distance of the curing light from the tooth surface, and thickness of the resin being cured.9 Because direct composite is inadequately cross-linked, the mechanical properties are not fully optimized, resulting in accelerated wear and a relatively weak fracture-toughness performance. One study that looked at the fracture toughness of 6 different direct resin materials found the average fracture toughness to be around 1 KIc.10 This is far lower compared to natural tooth structure, which has a fracture toughness of around 2 KIc.11 Fracture toughness values are extremely important, and in a recent systematic review, fracture toughness was the test that most closely correlated with clinical longevity.12 The fracture toughness of Ceramic Crown material (SprintRay) is 2.1 KIc, which is very close to natural tooth structure.
Three-dimensionally printed resins have incredible mechanical properties due to their novel polymer chemistry and functionalized filler particles that are cured using high heat and powerful ultraviolet sources according to validated protocols. This enables 3D printed restorations to achieve above 90% bond conversion, significantly improving strength and wear resistance while not inhibiting long-term bond strength.13 In a recent study, 3D printed denture teeth outperformed premium carded denture teeth in simulated wear testing against zirconia antagonists.14
Another significant disadvantage of direct resin is polymerization shrinkage stress. Direct resins cured in situ have been shown to generate stress on the walls of the preparation due to polymer-
ization shrinkage. This is suspected to contribute to mechanical failure of direct restorations and can also cause gap formation resulting in microleakage and recurrent decay. Indirect resin restorations have been shown to almost eliminate this stress completely on the bond as any polymerization shrinkage happens extraorally and luting resin fills any voids between the restoration and preparation walls.15,16
Due in part to fabrication and material performance challenges, only 6% of dental restorative treatments in the United States involve inlays and onlays. Milled composites were promised as an ideal material in these indications but unfortunately suffered from common debonding issues and high-water uptake, based in part on their old legacy resin chemistry. These debonding failures occur with milled resin partially due to the complete bond conversion within their polymer structures. The lack of residual methacrylate groups makes these materials difficult to bond, resulting in adhesive failures at the luting interface.17,18 Furthermore, many milled resins are based on older resin chemistry from the 1950s, leading to accelerated water uptake that further exasperated deboning issues clinically.19 Contrastingly, studies have demonstrated that bonding to 3D printed restorations exhibits excellent initial bond strength that actually increases over time.20
Several novel 3D printing materials, such as Ceramic Crown resin, contain greater than 50% ceramic nanoparticles, enabling them to meet ADA requirements for definitive ceramic restorations. As such, these can be billed using CDT codes previously reserved for zirconia or lithium disilicate. Ceramic Crown resin is an FDA-cleared Class II resin for 3D printing definitive full crowns, inlays/onlays, and veneers. The material has high strength and wear resistance, and it is radiopaque for clear visibility on radiographs for monitoring during routine recall appointments. The resin has a flexural strength of 150 +/- 25 MPa, which is comparable to leucite glass ceramics (150 MPa), and its shear bond strength is comparable to lithium disilicate.21 Ceramic Crown resin has a very low water absorption, reducing its tendency to age and stain, while its smooth surface minimizes plaque accumulation.
In the presented case, 3D printing enabled a full quadrant of inlay/onlay restorations to be prepped, designed, and delivered within a single 2-hour visit. In a team-driven approach, the scanning, design, and restoration fabrication were all performed by an assistant. This is a significant time savings compared to direct composite restorations where a full quadrant might take a full hour of meticulous attention by the clinician. Three-dimensional printing facilitates single-appointment inlay/onlay restorations with a workflow that can largely be delegated to the team.
CASE REPORT
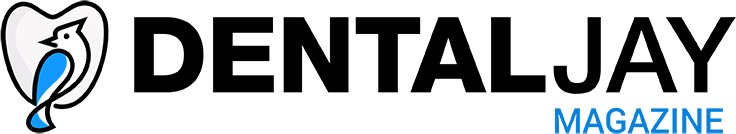
A 35-year-old female patient presented for a routine prophylaxis appointment after an 18-month delay due to the pandemic and other factors. During the hygiene appointment, she indicated sensitivity on the posterior left mandibular teeth that had been present for some time. Examination of the bite-wing radiographs taken at the appointment demonstrated recurrent decay associated with the restorations in teeth Nos. 18 to 20. A clinical exam noted tooth No. 18 had a large MO amalgam with marginal breakdown on the occlusal surface and recurrent decay. Tooth No. 19 had separate DO and MO amalgam restorations with a dark area under the central fossa, and a crack was noted in the mid-buccal extending from the gingival margin to the area noted at the central fossa. Tooth No. 20 had an MOD composite restoration with dark shading on the distal occlusal and marginal breakdown on the mesial portion (Figure 1). The patient indicated that she would be traveling in a few days and inquired if the treatment could be done that day and completed before her trip. Based on the clinical findings, the patient opted for single-visit delivery of inlay/onlays on teeth Nos. 18 to 20 utilizing in-office 3D printing. She was informed that the crack on tooth No. 19 may necessitate a larger restoration, but that would be determined following the removal of the current restorations and decay. The patient agreed to treatment, and treatment was initiated.
Figure 1. Clinical presentation of a failing MOD composite in tooth No. 20, MO and DO amalgams in No. 19, and a large MO amalgam in No. 18.
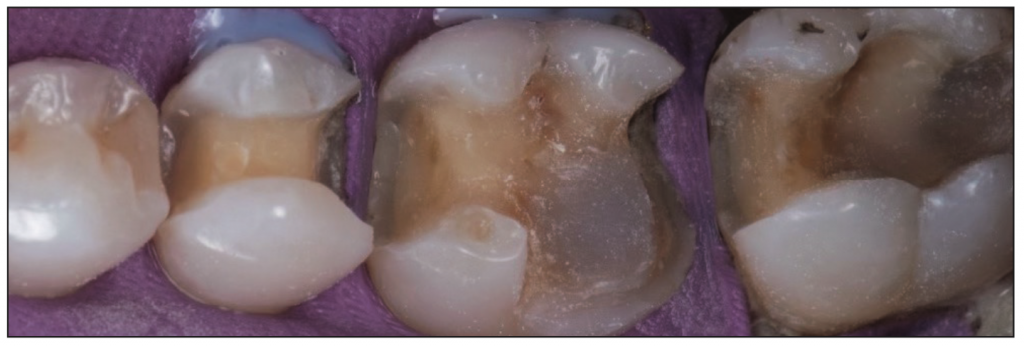
Figure 2. Clinical picture following removal of the failing restorative material and decay with preparation for inlay restorations on Nos. 18 and 20 with an onlay on tooth No. 19.
Local anesthetic was placed using an IAN block and mental injection. A rubber dam was applied, and the amalgam and composite were removed from the teeth with a carbide bur in a high-speed handpiece. Due to the crack on the buccal aspect of No. 19, the distal-buccal cusp was compromised, which necessitated its removal from the tooth. No pulpal exposure was noted following removal of the cusp. Recurrent decay was removed from the 3 teeth, and an OM inlay was planned for No. 18, an MODB onlay was planned for No. 19, and an MOD inlay was planned for No. 20. Tetric EvoFlow (Ivoclar Vivadent), a flowable composite, was placed to block out any undercuts on the preparations and cover the pulpal floor at the missing cusp on No. 19. This was then light-cured, and the preparations were refined (Figure 2).
The procedure was handed off to the dental assistant to scan, design, and print the restorations. The rubber dam was removed, and the quadrant was scanned with an intraoral scanner (Primescan [Dentsply Sirona]) (Figure 3). Within exocad (exocad America), the restoration margins were identified, and offset parameters were set for a 120-µm cement gap with a margin ramp of 200 µm to generate the restorations (Figure 4). Printing would be performed on the Pro 55S 3D printer (SprintRay) utilizing A1 Ceramic Crown resin (SprintRay) with a 100-µm print layer height. The virtual design restorations were completed and ready to be printed (Figures 5 to 8).
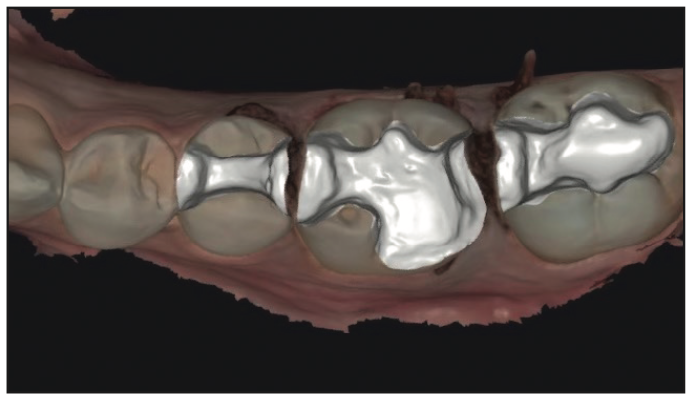
Figure 3. Virtual model of the prepared teeth ready for virtual design of the restorations in preparation for 3D printing.
Figure 4. The planned restorations have been virtually designed on teeth Nos. 18 to 20.
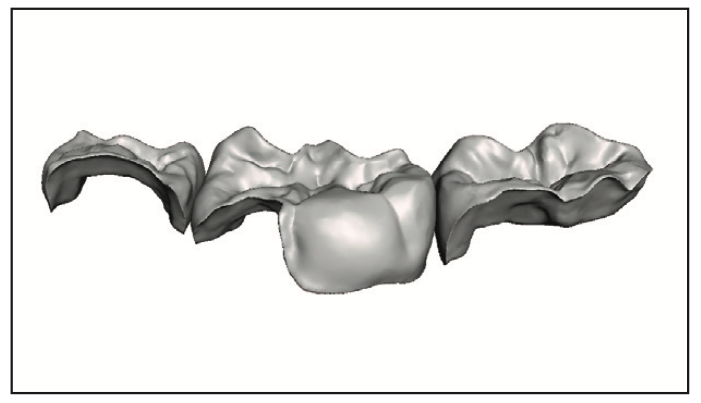
Figure 5. Buccal view of the individual restorations without the virtual model.
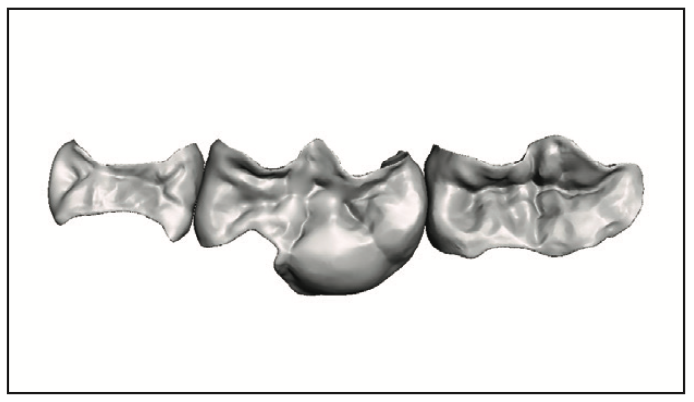
Figure 6. Occlusal view of the individual restorations without the virtual model.
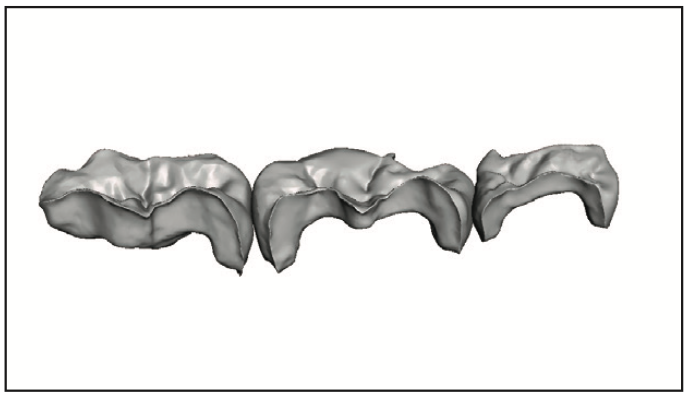
Figure 7. Lingual view of the individual restorations without the virtual model.
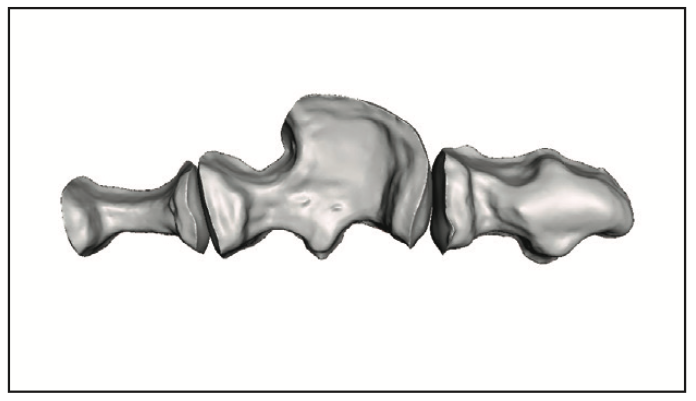
Figure 8. Intaglio view of the individual restorations without the virtual model.
The exported STL files for these restorations were imported into RayWare Cloud (SprintRay), where automated algorithms determined the print layout and support structures in 100-µm layers in crown mode using the crown kit, which would allow printing of the restorations in 10 minutes (Figures 9 and 10). RayWare is automated dental 3D printing software that takes the designs from exocad or other similar design software and sets it for printing in the various SprintRay printers available.
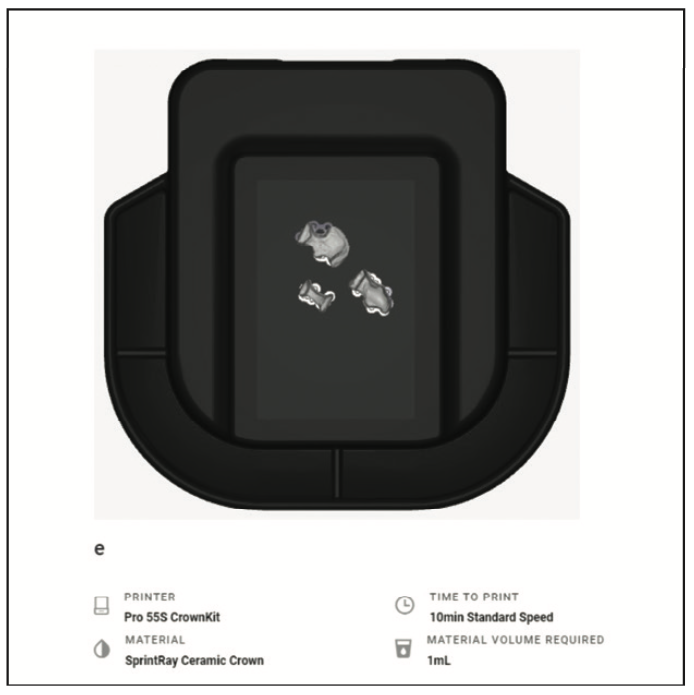
Figure 9. Planned restorations were placed on the build platform for preview in RayWare (SprintRay), and AI nesting with a final check was performed.
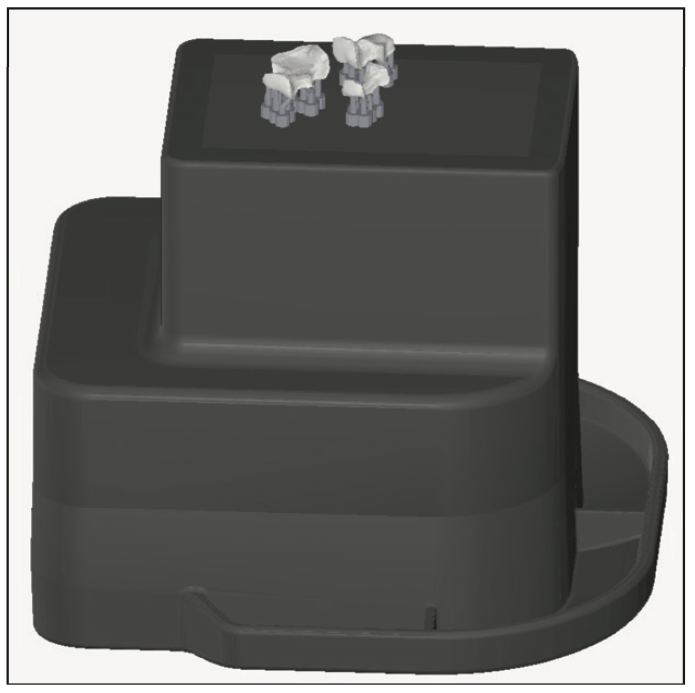
Figure 10. Side view on the virtual positioning of the restorations with supports on the build platform for preview in RayWare.
Following the printing of the restorations, which was accomplished in 10 minutes, the restorations were removed from the build platform and then spray washed for 20 seconds (Figure 11). The assistant then placed the restorations into the ProCure 2 unit (SprintRay) to cure the resin using the programmed settings, which was finished in 6 minutes. The ProCure 2 delivers a concentrated 385-nm light, which generates heat locally on each part, accelerating resin curing and thus decreasing processing time. The supports were removed from the restorations, and surfaces were polished to achieve the desired contours. The assistant next applied light staining to the pits and fissures to simulate a natural appearance using IPS Empress Direct Color (Ivoclar) and light cured the restorations. Then the restorations were taken to the operatory and trial-seated in the preparations to confirm fit, and the doctor was called back to the operatory.
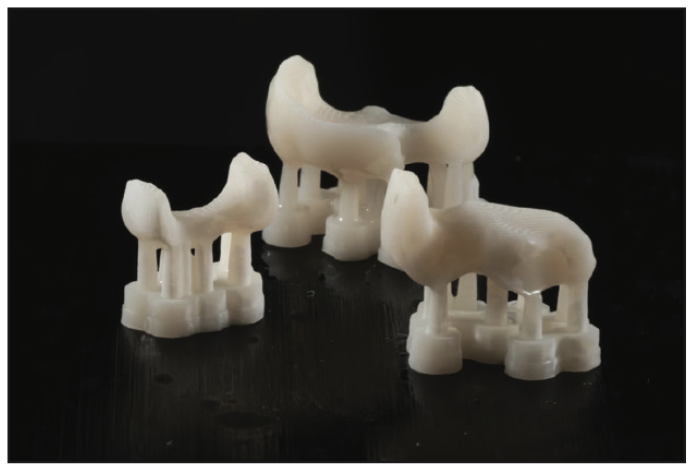
Figure 11. The restorations following 3D printing, with the supports present after separation from the plate, and ready for finishing.
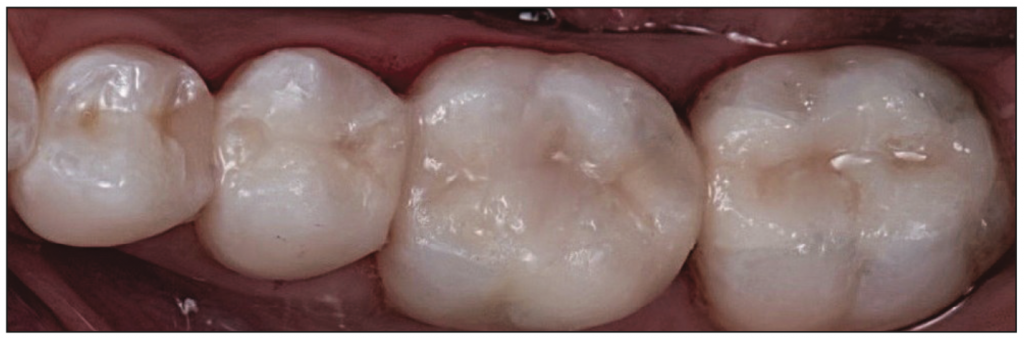
Figure 12. Restorations to the prepared teeth following luting and finishing of the margins after occlusal adjustment.
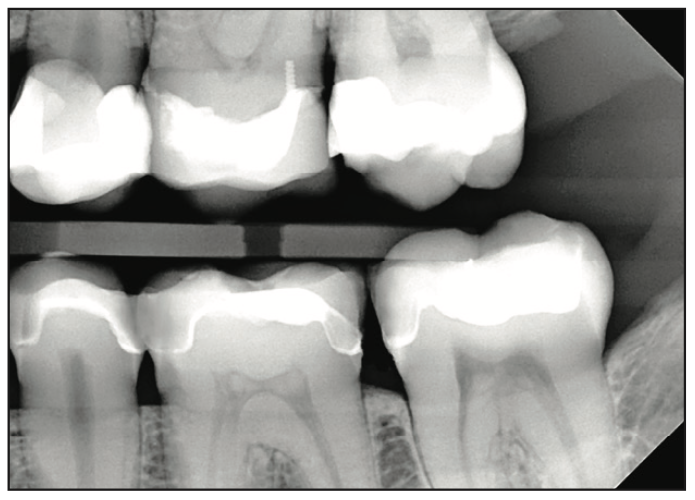
Figure 13. Radiograph of the luted restorations.
The doctor checked the proximal contacts of the restorations with floss and an explorer and also checked the marginal fit. The restorations were removed, and a rubber dam was placed. Selective etching with a 37% phosphoric acid gel was performed on the enamel margins. The interior of the restorations (intaglio surface) was treated by sandblasting it with 50-µm alumina oxide particles to roughen the surface and increase bondability. Adhese Universal adhesive (Ivoclar) was applied to the enamel, dentin, and resin blockout on the teeth and to the interior surfaces of the restorations and was not light-cured. Variolink Esthetic DC (Ivoclar), a light-cure and dual-cure luting composite for adhesive cementation of dental restorations, was applied to the preparation surfaces on the teeth. The restorations were then seated and tack-cured for 5 seconds for each tooth. The excess luting composite was cleared from the margins with a brush and interproximally with floss. The restorations were then light-cured from the occlusal, buccal, and lingual surfaces for 30 seconds per surface per tooth. The margins were checked for any residual luting resin with an explorer and floss. Occlusion was checked and did not require any adjustments (Figure 12). A bite-wing radiograph was taken to confirm fit and lack of residual luting resin (Figure 13). The cement layer between the intaglio surface of the restorations and the preparation was minimal, allowing the strength of the Ceramic Crown resin to provide maximum benefits and durability.
The restorations were placed a little more than one year ago, and on subsequent recall prophy appointments, one being at the one-year anniversary of restoration placement, demonstrated no occlusal or marginal wear. The patient reported no sensitivity at any point following restoration placement.
CONCLUSION
The benefit of in-office 3D printing is that restorations can be completed in a single visit, as demonstrated by the case presented. Although the total treatment time in the office was 2 hours, a majority of the work in that time was performed by trained staff, highlighting the effectiveness of team-driven care. The practitioner’s time involved preparation of the teeth and luting of the finished restorations—approximately 30 to 45 minutes of the total treatment time. Team members scanned the preparations, imported the data into the software, utilized the AI capabilities of the software to design the restorations, printed the restorations, finished them, and verified seating before having the practitioner lute those restorations. Thus, use of this approach provides practical care in a single visit without a large time involvement by the practitioner, freeing him or her to treat other patients while the restorations are being fabricated.
The Ceramic Crown resin has been shown to be a durable material with good wear characteristics that provides an aesthetic restoration without the need for involvement with an outside lab and the increase in costs and turnaround time involved. Additionally, patients ideally would like one-stop shopping where treatment can be accomplished in a single visit, freeing up their schedules for other parts of life, such as work and family.
REFERENCES
1. Zimmermann M, Ender A, Egli G, et al. Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin Oral Investig. 2019;23(6):2777–84. doi:10.1007/s00784-018-2717-2
2. Corbani K, Hardan L, Skienhe H, et al. Effect of material thickness on the fracture resistance and failure pattern of 3D-printed composite crowns. Int J Comput Dent. 2020;23(3):225–33.
3. Donovan TE. Longevity of the tooth/restoration complex: a review. J Calif Dent Assoc. 2006;34(2):122–8.
4. Dennison JB, Hamilton JC. Treatment decisions and conservation of tooth structure. Dent Clin North Am. 2005;49(4):825–45. doi:10.1016/j.cden.2005.05.007
5. Wayakanon K. Partially coverage restoration: an esthetically conservative treatment for a complex cavity restoration. Open J Stomatol. 2017;7(4):234–41. doi:10.4236/ojst.2017.74017
6. Opdam NJ, van de Sande FH, Bronkhorst E, et al. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res. 2014;93(10):943–9. doi:10.1177/0022034514544217
7. Bustamante-Hernández N, Montiel-Company JM, Bellot-Arcís C, et al. Clinical behavior of ceramic, hybrid, and composite onlays. A systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(20):7582. doi:10.3390/ijerph17207582
8. Ribeiro BC, Boaventura JM, Brito-Gonçalves Jd, et al. Degree of conversion of nanofilled and microhybrid composite resins photo-activated by different generations of LEDs. J Appl Oral Sci. 2012;20(2):212–7. doi:10.1590/s1678-77572012000200015
9. Barakah H. Effect of different curing times and distances on the microhardness of nanofilled resin-based composite restoration polymerized with high-intensity LED light curing units. Saudi Dent J. 2021;33(8):1035–41. doi:10.1016/j.sdentj.2021.05.007
10. Watanabe H, Khera SC, Vargas MA, et al. Fracture toughness comparison of six resin composites. Dent Mater. 2008;24(3):418–25. doi:10.1016/j.dental.2007.06.018
11. Yahyazadehfar M, Ivancik J, Majd H, et al. On the mechanics of fatigue and fracture in teeth. Appl Mech Rev. 2014;66(3):0308031-3080319. doi:10.1115/1.4027431
12. Heintze SD, Ilie N, Hickel R, et al. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials—a systematic review. Dent Mater. 2017;33(3):e101-e114. doi:10.1016/j.dental.2016.11.013
13. Lim JH, Lee SY, Gu H, et al. Evaluating oxygen shielding effect using glycerin or vacuum with varying temperature on 3D printed photopolymer in post-polymerization. J Mech Behav Biomed Mater. 2022;130:105170. doi:10.1016/j.jmbbm.2022.105170
14. Pham DM, Gonzalez MD, Ontiveros JC, et al. Wear resistance of 3D printed and prefabricated denture teeth opposing zirconia. J Prosthodont. 2021;30(9):804–10. doi:10.1111/jopr.13339
15. Dejak B, Młotkowski A. A comparison of stresses in molar teeth restored with inlays and direct restorations, including polymerization shrinkage of composite resin and tooth loading during mastication. Dent Mater. 2015;31(3):e77-87. doi:10.1016/j.dental.2014.11.016
16. Ausiello P, Ciaramella S, Fabianelli A, et al. Mechanical behavior of bulk direct composite versus block composite and lithium disilicate indirect Class II restorations by CAD-FEM modeling. Dent Mater. 2017;33(6):690-701. doi:10.1016/j.dental.2017.03.014
17. Wierichs RJ, Kramer EJ, Reiss B, et al. A prospective, multi-center, practice-based cohort study on all-ceramic crowns. Dent Mater. 2021;37(8):1273–82. doi:10.1016/j.dental.2021.04.005
18. Awad MM, Albedaiwi L, Almahdy A, et al. Effect of universal adhesives on microtensile bond strength to hybrid ceramic. BMC Oral Health. 2019;19(1):178. doi:10.1186/s12903-019-0865-7
19. Schepke U, Filius D, Lohbauer U, et al. Dimensional changes of CAD/CAM polymer crowns after water aging—an in vitro experiment. J Mech Behav Biomed Mater. 2022;128:105109. doi:10.1016/j.jmbbm.2022.105109
20. Lankes V, Reymus M, Liebermann A, et al. Bond strength between temporary 3D printable resin and conventional resin composite: influence of cleaning methods and air-abrasion parameters. Clin Oral Investig. 2023;27(1):31-43. doi:10.1007/s00784-022-04800-7
21. Jurado CA, Ahmed AS, Lawson NC, et al. Fracture resistance of zirconia surveyed crowns with four different occlusal rest seat designs. J Prosthodont. 2023. doi:10.1111/jopr.13737.
ABOUT THE AUTHORS
Dr. Renne is the founder of the MOD Institute, where he instructs clinicians on the application of the latest digital technologies with a focus on minimal prep techniques to preserve natural dentition. With 3 years of dental 3D printing experience, he has delivered more than 1,000 printed restorations, including veneers, inlays, onlays, and crowns. Dr. Renne can be reached at dr.renne@themodinstitute.com.
Dr. Kurtzman is in private general dental practice in Silver Spring, Md, a former assistant clinical professor at the University of Maryland in the Department of Restorative Dentistry and Endodontics, and a former American Academy of Implant Dentistry Implant MaxiCourse assistant program director at the Howard University College of Dentistry. He has lectured internationally on the topics of restorative dentistry, endodontics, implant surgery, prosthetics, removable and fixed prosthetics, and periodontics and has published more than 830 articles globally, as well as several e-books and textbook chapters. He has earned Fellowship in the AGD; American College of Dentists; International Congress of Oral Implantology (ICOI); Pierre Fauchard Academy; Academy of Dentistry International; and the International Academy of Dental Facial Esthetics, Mastership in the AGD and ICOI; and Diplomate status in the ICOI, American Dental Implant Association, and the International Dental Implant Association. Dr. Kurtzman has been honored to be included in Dentistry Today’s Leaders in CE listings annually since 2006. He can be reached via email at dr_kurtzman@maryland-implants.com.
Disclosure: Dr. Renne reports no disclosures. Dr. Kurtzman received compensation for writing this article.