INTRODUCTION
Milled/sintered materials like zirconia and IPS e.max (Ivoclar Vivadent) are the industry standard for crowns. But these materials have demonstrated accelerated wear on opposing dentition over time due to their greater hardness and abrasive nature compared to enamel. Alternative milled materials, such as IPS Empress (Ivoclar Vivadent), are often preferred due to their wear characteristics being more comparable to enamel, dentin, and composite.
Three-dimensionally printed materials have seen increased usage in recent years in various prosthetic and restorative treatment areas, either fabricated at the lab or in-office. Novel 3D printed materials offer comparable mechanical performance to natural dentin and demonstrate comparable wear as natural tooth to natural tooth. A study was performed to evaluate SprintRay Ceramic Crown resin intraorally (in vivo) on 25 single posterior and anterior crowns over a period of 9 months. No failures, material fractures, or excessive wear were noted in the study crowns.
When comparing various materials that may be utilized for a crown, flexural strength and flexural modulus need to be compared to dentin as the bulk of the tooth is dentin (Table 1). Following preparation, there could be minimal or no remaining enamel on the tooth. Additionally, the restoration is cemented or bonded to the dentin, replacing the enamel removed during preparation. Dentin has been reported to have a flexural strength of 150 to 250 MPa and a flexural modulus of 12 to 21 GPa.1,2
Table 1. Flexural strength and modulus of the SprintRay Ceramic Crown and various ceramic restorative materials compared to dentin.
Zirconia is a very strong material with a reported flexural strength of approximately 1,000 MPa when veneered with another ceramic3 and approximately 1,200 MPa when monolithic.4 A flexural modulus of 210 GPa has been reported for this material. Unfortunately, it has also been reported to increase wear on opposing teeth, which is dependent on the polish of the restoration and the patient’s bruxism habits.5,6 If any adjustments are needed to adjust the occlusion, it is recommended that proper polishing is performed so that a rough area that may accelerate wear is not present.
IPS e.max, a lithium disilicate glass ceramic, has become a common milled or sintered ceramic for crowns and other single-unit restorations. A flexural strength of 250 MPa and a flexural modulus of 80 GPa has been reported.7 Restorations made from this material may demonstrate wear on opposing dentition but less than zirconia. As the material is stiffer than dentin, a fracture may occur under heavy functional loading or in patients who brux. Pressed IPS e.max has been reported to have more issues than milled restorations of this material.8 The fracture resistance of fully crystallized lithium disilicate ceramic block materials is lower than their pre-crystallized counterparts. So the handling of the milled restorations during fabrication affects their fracture resistance and long-term survival.9 When the material has been subjected to aging, increased surface roughness and microstructure alterations have been observed. This may increase wear of the opposing dentition and also lead to fracturing of the crown material, especially when it is thin.10
IPS Empress, a leucite glass ceramic, has been in use prior to IPS e.max for single-unit restorations. A flexural strength of 150 MPa and a flexural modulus of 32 GPa has been reported.11 As its mechanical properties are lower than IPS e.max, this material has been utilized to preserve surrounding dentition and minimize antagonist wear.
Printed restorations have increasingly been replacing CAD-milled restorations over the past few years due to their easier fabrication process, with an annual growth of 20%.12 Ceramic resins have been introduced to be used with printers as a more durable material for restorations than previously used print resins.
VarseoSmile Crown plus (BEGO), a ceramic-filled resin that is printed for permanent crowns, has a reported flexural strength of 116 MPa and a flexural modulus of 4.1 GPa, which is significantly lower than dentin.13 This mismatch of mechanical properties with dentin poses a significant risk of fracture in the long term, especially in those patients who brux.
SprintRay Ceramic Crown is an FDA-cleared Class II resin for printing definitive crown restorations. The material has received FDA 510(k) approval for definitive and fixed full single anterior and posterior crowns, definitive partial crowns (onlays and crownlays), and single veneers. It may also be used to produce artificial teeth for dentures and monolithic full and partial dentures. This new, ceramic-filled 3D-print resin with improved strength values has a flexural strength of 136 MPa and a flexural modulus of 7.5 GPa due to its ceramic filler content (>51% by mass). The material is radiopaque for clear radiographic visibility. It possesses a high composite bond strength (the bond between the prosthetic and natural tooth surface), reducing the likelihood of secondary caries and failures. Low water absorption and water solubility provide a restorative material with a low tendency to discolor due to the liquids and foods the patient may eat. The resin is available in A1, A2, A3, B1, B3, C2, D3, and bleach shades to fit the patient shade values needed.
CASE STUDIES
Case 1
A 25-year-old male patient presented with discomfort on tooth No. 2 (maxillary right second molar). A radiograph was taken, and decay was noted on the mesial with pulpal involvement (Figure 1). Endodontics was recommended, followed by a full-coverage crown. Following endodontic treatment, a resin-bonded core buildup was placed, and the tooth was prepared for a full-coverage crown. The preparation was scanned using Primescan (Dentsply Sirona) (Figure 2). The restoration was temporized, and the patient was appointed the next day to insert the final restoration. The scan data was imported into inLab CAD design software (Dentsply Sirona), and a full-coverage crown was designed for tooth No. 2 (Figure 3). The definitive crown was printed using SprintRay Ceramic Crown resin on the SprintRay 55 printer, then finished and polished, and then it was ready for insertion. The process was completed in less than 30 minutes, with the crown taking less than 10 minutes.
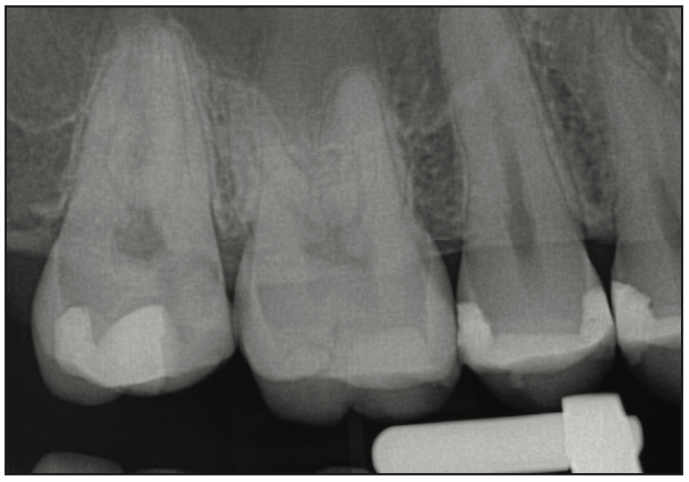
Figure 1. Pretreatment radiograph demonstrating caries on tooth No. 2 on the mesial with pulpal involvement.
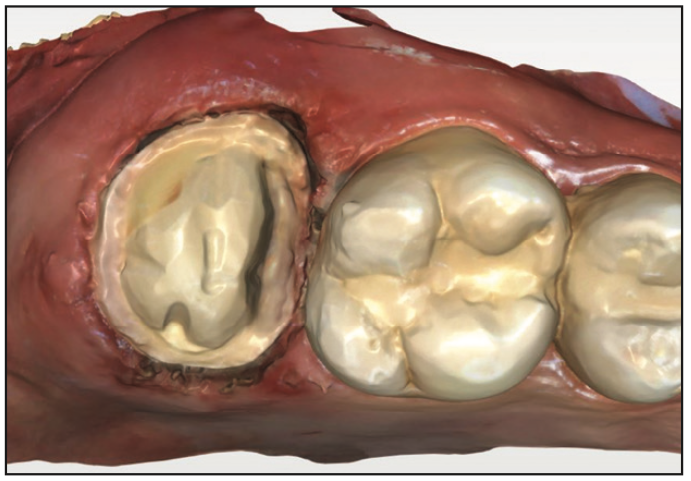
Figure 2. Intraoral scan following crown preparation after endodontic treatment and core buildup on tooth No. 2.
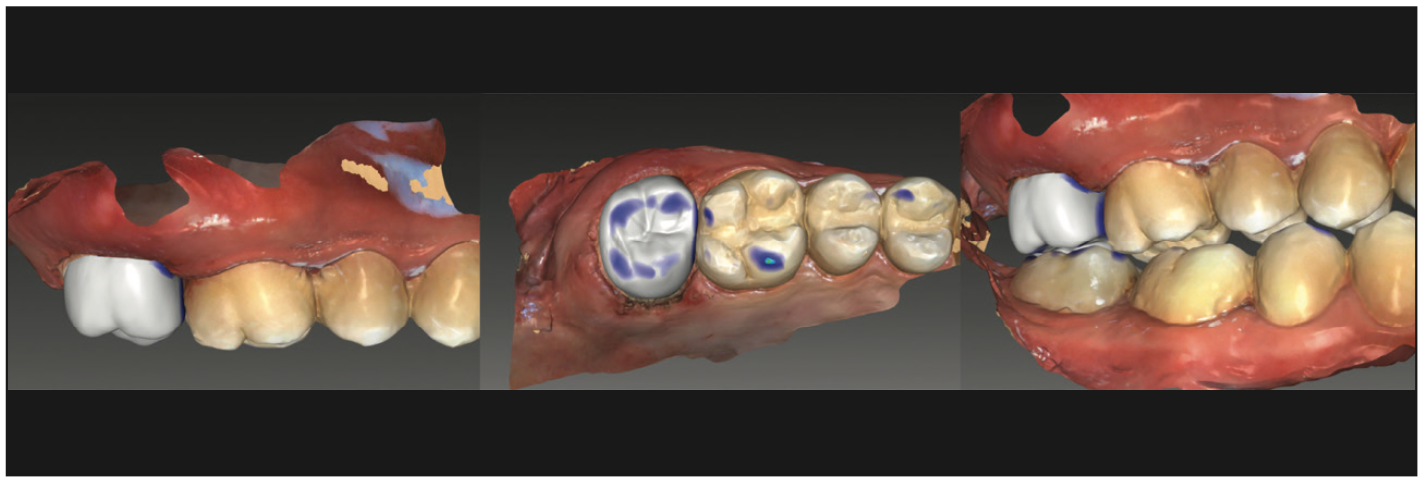
Figure 3. Virtual crown to be printed on the SprintRay 55 printer and designed in inLab software (Dentsply Sirona).
As a comparison for the fit of the printed SprintRay Ceramic Crown, an IPS e.max crown was milled as well. Following the milling of both crowns, upon comparison, the exteriors looked similar, presenting as a polished restoration with matching anatomical detail (Figure 4). Yet, the intaglio surface of the printed SprintRay Ceramic Crown had a rougher surface than the IPS e.max crown, which would improve restoration retention to the preparation (Figure 5).
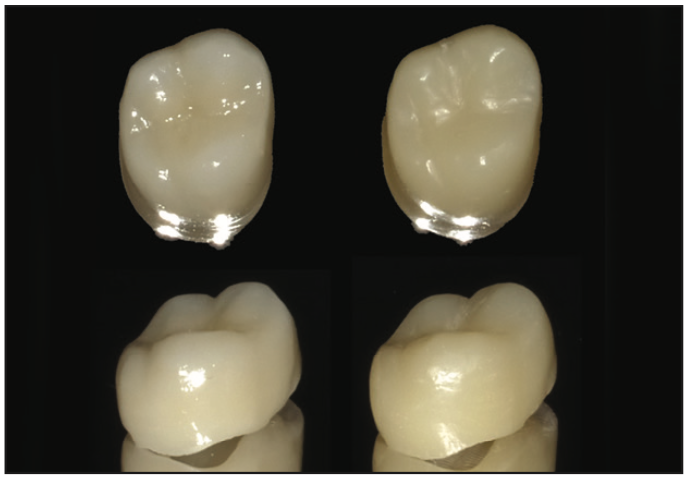
Figure 4. Views of the IPS e.max (Ivoclar Vivadent) milled crown (left) and printed SprintRay Ceramic Crown restoration (right).
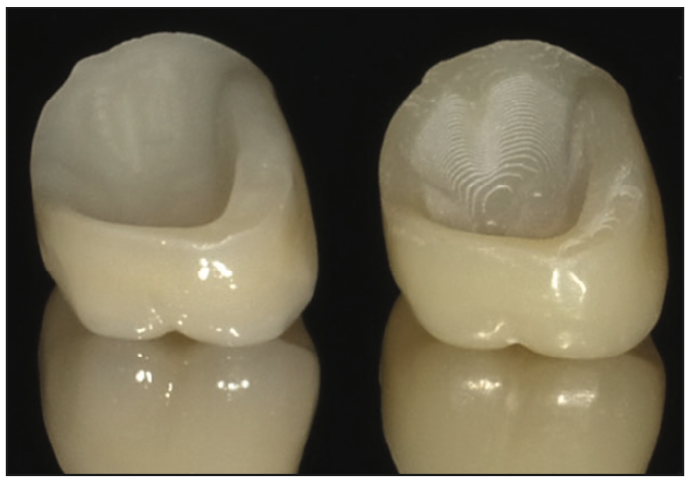
Figure 5. View of the tooth side of the IPS e.max milled crown (left) and printed SprintRay Ceramic Crown (right). The printed ceramic resin restoration demonstrated a rougher surface on the printed crown, which improved cementation adherence to the crown material compared to the milled surface.
The patient returned the next day, the provisional crown was removed, and any residual temporary cement was cleaned up in preparation for the final restoration placement. Both crowns, the IPS e.max crown and the SprintRay Ceramic Crown, were tried in to check fit and marginal integrity. Marginal adaption and integrity was found to be identical between the 2 crowns. But the SprintRay Ceramic Crown restoration appeared to have better retention to the preparation when lateral light force was placed on the uncemented crowns. A periapical radiograph was taken of the SprintRay Ceramic Crown restoration on the preparation to check the fit, and good marginal adaption was noted (Figure 6, left). Multilink Primers A and B (Ivoclar Vivadent) were dispensed into a dish and mixed, then applied to the preparation. Monobond Etch & Prime (Ivoclar Vivadent) was applied to the intaglio surface of the SprintRay Ceramic Crown restoration, and the crown was filled with Multilink Dual-Cure Resin Cement (Ivoclar Vivadent) and then seated intraorally on the preparation. Excess resin cement was removed with a brush wetted with Monobond, and the restoration was light cured and then allowed to self-cure. Following curing, the margins were checked for residual cement, and the occlusion was checked. A periapical radiograph was taken to confirm restoration fit and adaption to the preparation (Figure 6, right). A post-insertion scan was taken with Primescan for study purposes (Figure 7).
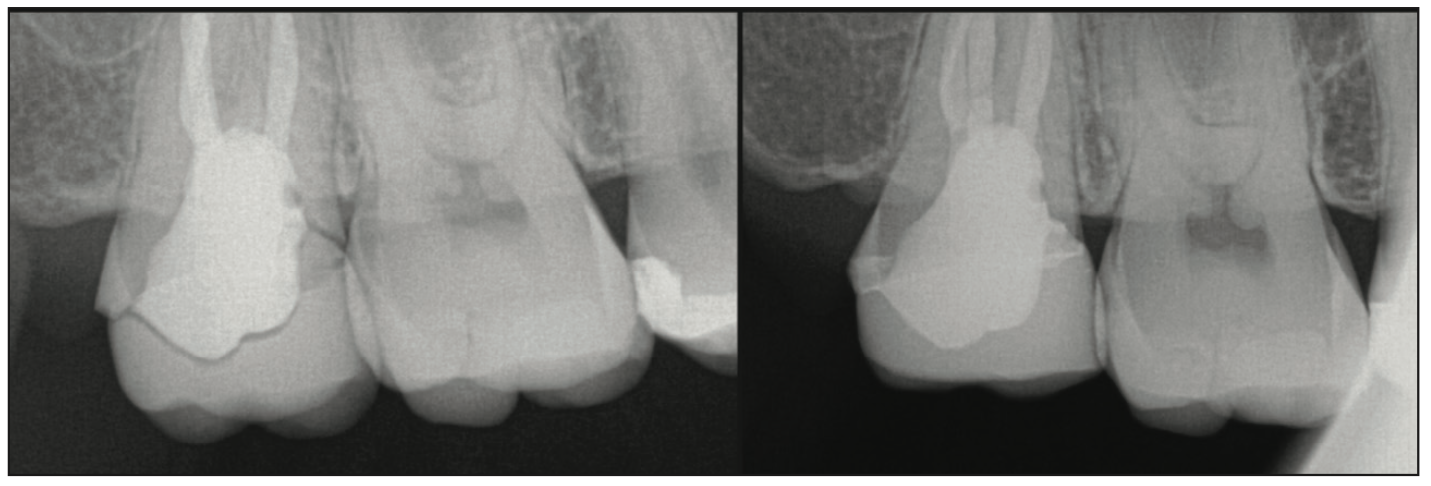
Figure 6. Radiographs at the try-in of the printed SprintRay Ceramic Crown restoration (left) and following cementation (right).
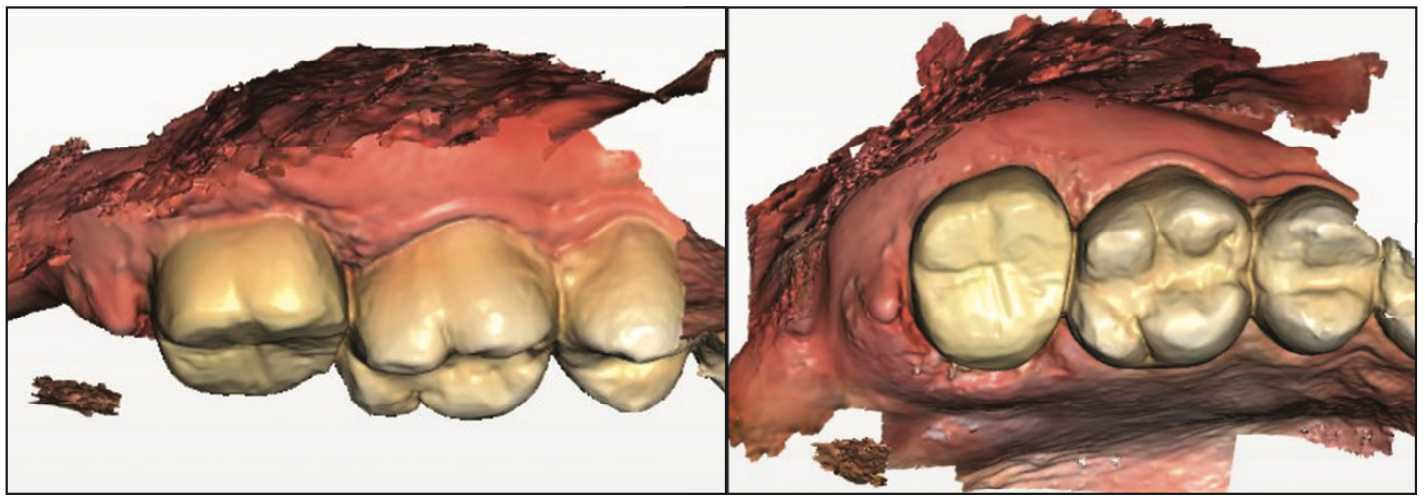
Figure 7. Post-insertion intraoral scan of the SprintRay Ceramic Crown restoration on tooth No. 2.
Case 2
A 66-year-old female patient presented for recall prophylaxis and had radiographs taken, which noted recurrent marginal decay on the PFM crown on tooth No. 29 (Figure 8). The patient was informed that the crown would require replacement due to the recurrent decay. The crown was removed following administration of local anesthetic, and the preparation was refined to remove the decay noted. The preparation was scanned using Primescan (Figure 9). The scan data was imported into the inLab CAD software, and the virtual crown was designed for printing (Figure 10). The definitive crown was printed using SprintRay Ceramic Crown resin on the SprintRay 55 printer, then it was finished and polished and ready for insertion (Figure 11).
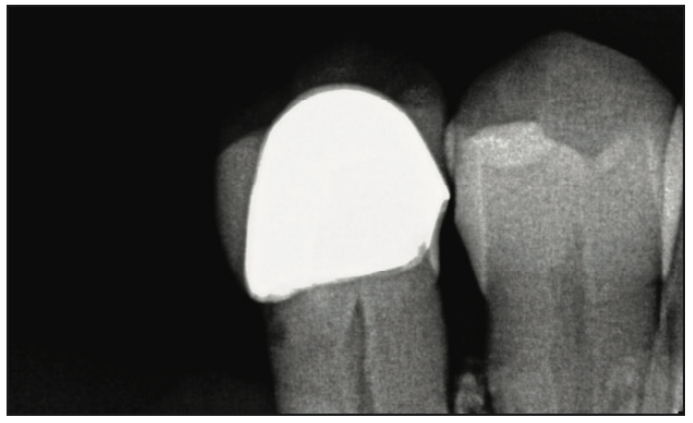
Figure 8. Radiograph demonstrating marginal caries at the PFM crown on No. 29.
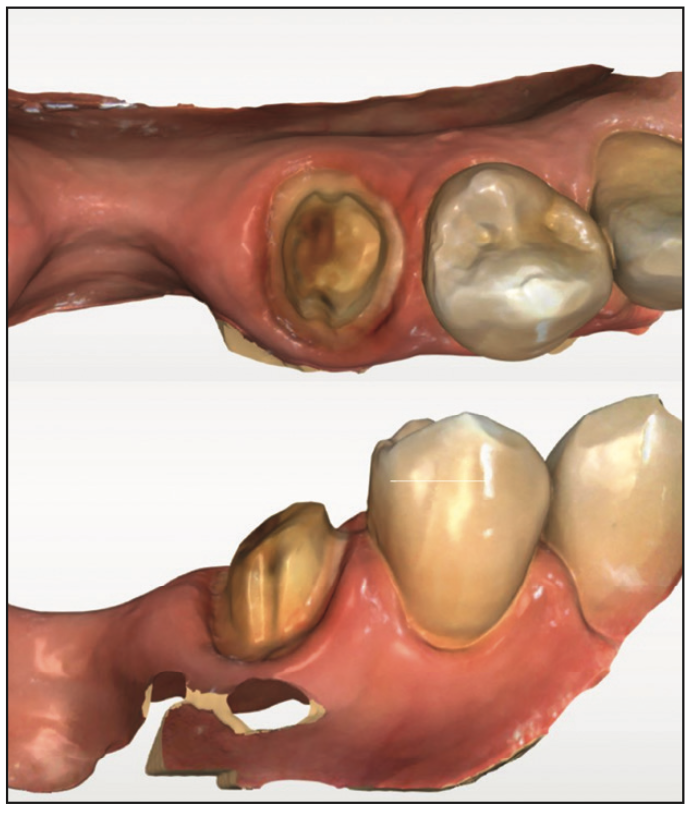
Figure 9. Following removal of the failing crown, the preparation was refined to remove caries and scanned for crown fabrication.
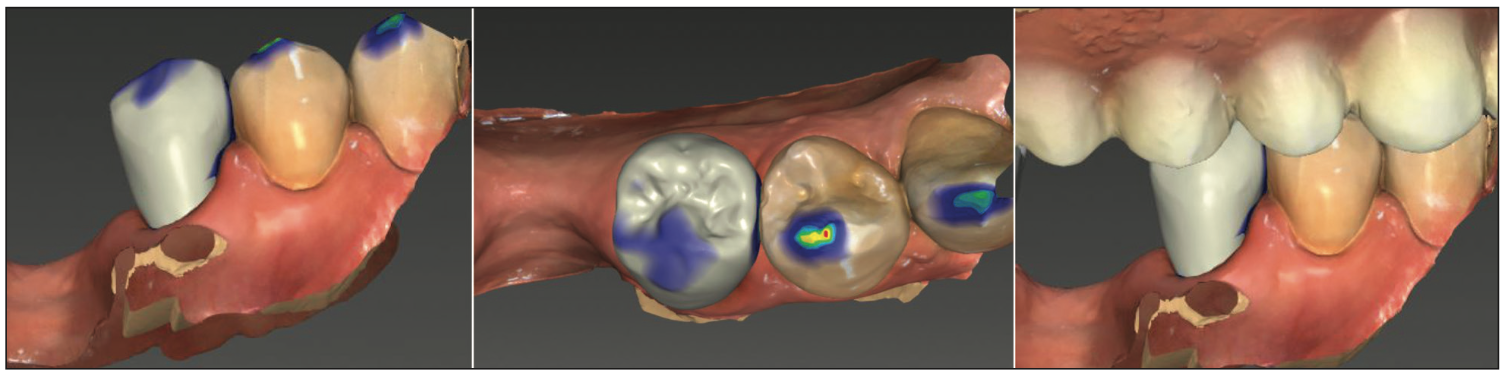
Figure 10. The virtual crown to be printed on the SprintRay 55 printer and designed in inLab CAD software.

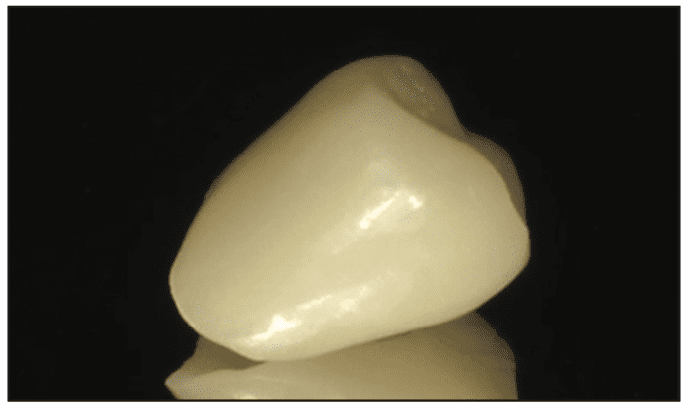
Figure 11. The printed crown made using SprintRay Ceramic Crown resin, following finishing and polishing and ready for intraoral insertion.
The printed crown was tried in for marginal adaption, and integrity was checked with an explorer. A periapical radiograph was taken of the SprintRay Ceramic Crown restoration on the preparation to check the fit, and good marginal adaption was noted (Figure 12, left). The same cementation process was utilized as was performed in case 1. Multi-link Primer A+B was applied to the preparation, with Monobond Etch & Prime applied to the intaglio surface of the SprintRay Ceramic Crown restoration. Multilink dual-cure resin cement was then utilized to lute the crown to the preparation. A periapical radiograph was taken to confirm restoration fit and adaption to the preparation (Figure 12, right). Clinically, the printed crown had good anatomical features and adaptation to the tooth at the margins (Figures 13 and 14).
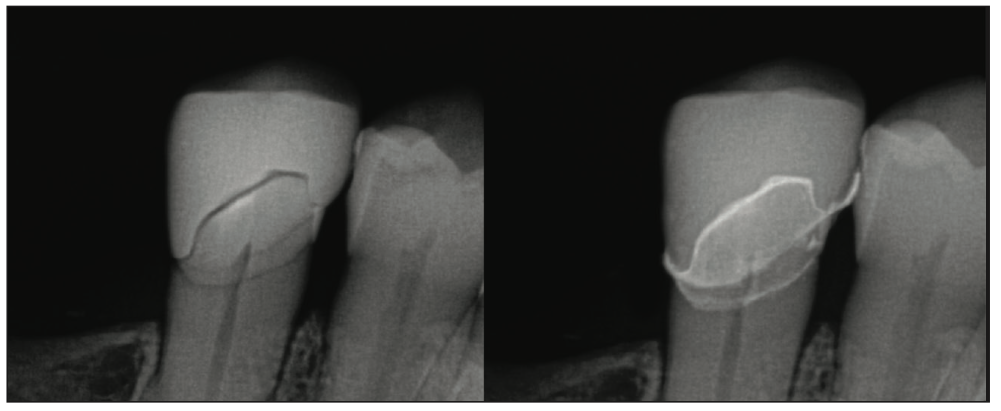
Figure 12. Radiograph at try-in of the SprintRay Ceramic Crown printed restoration on No. 29 (left) and following cementation (right).

Figure 13. Final 3D-printed crown using SprintRay Ceramic Crown resin, following cementation, as shown from the occlusal view.

Figure 14. Final 3D-printed crown using SprintRay Ceramic Crown resin, following cementation, as shown from the buccal view.
CONCLUSION
These 2 case examples illustrate crowns printed with SprintRay Ceramic Crown and had a good final polish with marginal adaption similar to ceramic milled/sintered materials. These 2 cases, as well as the other cases in the study, were followed for 6 months or longer, and no noticeable wear was noted on the crown resin or opposing dentition. No fractures were noted in the material in any of the cases, demonstrating that SprintRay Ceramic Crown is a viable material for single crowns and should be considered when planning these types of restorations.
ACKNOWLEDGMENT
The authors wish to thank Henna Lee for the in-office lab work for the 2 cases presented.
REFERENCES
1. Plotino G, Grande NM, Bedini R, et al. Flexural properties of endodontic posts and human root dentin. Dent Mater. 2007;23(9):1129–35. doi:10.1016/j.dental.2006.06.047
2. Marending M, Paqué F, Fischer J, et al. Impact of irrigant sequence on mechanical properties of human root dentin. J Endod. 2007;33(11):1325–8. doi:10.1016/j.joen.2007.08.005
3. Tangsatchatham S, Juntavee N. Flexural strength of various types of computerized machinable ceramic veneered to yttria stabilized tetragonal zirconia polycrystalline ceramic upon different hybridized techniques. Clin Cosmet Investig Dent. 2019;11:61-71. doi:10.2147/CCIDE.S196297
4. Kontonasaki E, Giasimakopoulos P, Rigos AE. Strength and aging resistance of monolithic zirconia: an update to current knowledge. Jpn Dent Sci Rev. 2020;56(1):1-23. doi:10.1016/j.jdsr.2019.09.002
5. Aljomard YRM, Altunok EÇ, Kara HB. Enamel wear against monolithic zirconia restorations: A meta-analysis and systematic review of in vitro studies. J Esthet Restor Dent. 2022;34(3):473–89. doi:10.1111/jerd.12823
6. Gou M, Chen H, Kang J, et al. Antagonist enamel wear of tooth-supported monolithic zirconia posterior crowns in vivo: A systematic review. J Prosthet Dent. 2019;121(4):598-603. doi:10.1016/j.prosdent.2018.06.005
7. Al-Thobity AM, Alsalman A. Flexural properties of three lithium disilicate materials: An in vitro evaluation. Saudi Dent J. 2021;33(7):620–7. doi:10.1016/j.sdentj.2020.07.004
8. AbuHaimed TS, Alzahrani SJ, Farsi SA, et al. The effect of repeated pressing on the flexural strength, color stability, vickers hardness, and surface topography of heat-pressed lithium disilicate. Materials (Basel). 2022;15(19):6787. doi:10.3390/ma15196787
9. Jurado CA, Lee D, Cortes D, et al. Fracture resistance of chairside CAD/CAM molar crowns fabricated with different lithium disilicate ceramic materials. Int J Prosthodont. 2022. doi:10.11607/ijp.7802
10. Kim SH, Choi YS, Kang KH, et al. Effects of thermal and mechanical cycling on the mechanical strength and surface properties of dental CAD-CAM restorative materials. J Prosthet Dent. 2022;128(1):79-88. doi:10.1016/j.prosdent.2020.11.014
11. Awada A, Nathanson D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J Prosthet Dent. 2015;114(4):587–93. doi:10.1016/j.prosdent.2015.04.016
12. Barbella M. Dental 3D printing market is expanding 20% annually. Orthopedic Design and Technology. August 12, 2022.
13. Grzebieluch W, Kowalewski P, Grygier D, et al. Printable and machinable dental restorative composites for CAD/CAM application-comparison of mechanical properties, fractographic, texture and fractal dimension analysis. Materials (Basel). 2021;14(17):4919. doi:10.3390/ma14174919
ABOUT THE AUTHORS
Dr. Jockin practices oral implantology in Tampa, Fla, and serves as adjunct clinical faculty in the department of prosthodontics at the University of Florida College of Dentistry in Gainesville. She is founder of fullarchsuccess.com, director of wellness at Heartland Dental, and lectures nationwide on diverse topics ranging from full-mouth rehabilitation to wellness for the dental team. She can be reached at sjockin@gmail.com.
Disclosure: Dr. Jockin reports no disclosures.
Dr. Kristallis holds an academic adjunct faculty position in the department of head and neck surgery and plastic surgery at the University of California, San Diego (UC San Diego). He is the founder of San Diego Dental Health Center, LLC, a private practice with the UC San Diego Medical Center that specializes in oral and maxillofacial reconstruction, and a former faculty member at the University of California, Los Angeles School of Dentistry in the department of advanced prosthodontics and maxillofacial prosthodontics. He also maintained a private multispecialty group dental practice in Beverly Hills, Calif. His current focus is on developing integrated clinical digital dentistry protocols as they relate to implant, restorative, and reconstructive dentistry, and he is a Fellow of the Royal College of Dentists of Canada in prosthodontics. Dr. Kristallis is a consultant to numerous dental manufacturing companies regarding biomaterials, dental implants, and CAD/CAM technology. He can be reached at tkristalis@aol.com.
Disclosure: Dr. Kristallis is a paid consultant for SprintRay.
Dr. Kurtzman is in private general dental practice in Silver Spring, Md. He is a former assistant clinical professor at the University of Maryland in the department of restorative dentistry and endodontics and a former American Academy of Implant Dentistry Implant MaxiCourse assistant program director at the Howard University College of Dentistry. He has lectured internationally on the topics of restorative dentistry, endodontics, implant surgery, prosthetics, removable and fixed prosthetics, and periodontics and has published more than 800 articles globally as well as several ebooks and textbook chapters. Dr. Kurtzman has been honored to be included in Dentistry Today’s Leaders in CE listings annually since 2006. He can be reached at dr_kurtzman@maryland-implants.com.
Disclosure: Dr. Kurtzman reports no disclosures.