Ciro Gilvetti and Andrew Osafo detail the signs and symptoms of mouth cancer, and explain how to perform a mouth, head and neck cancer examination.
The past 19 months have been extremely challenging due to the COVID-19 pandemic. In spite of this, it is important that we do not forget about the other ‘big C’ – cancer.
Mouth cancer is a serious and debilitating disease that can devastate lives and prematurely end them. As dental professionals, we are in a prime position to raise awareness of mouth cancer and educate the public about this devastating condition. Are we doing this?
This article will review the signs and symptoms of mouth cancer, discuss how to perform a mouth, head and neck cancer examination and highlight some ways to raise awareness of mouth cancer.
Signs and symptoms of mouth cancer
The signs and symptoms of mouth cancer include:
- Persistent pain in the mouth
- White or red patches in the mouth
- A sore or ulcer in the mouth that does not heal within three weeks
- Lumps and swellings in the mouth, head or neck
- Difficulty in chewing or moving the tongue or jaw
- Chronic hoarseness or sore throat that persists more than six weeks
- Unexplained tooth mobility.
Almost all mouth cancers are preceded by visual changes of the oral mucosa (Mignogna et al, 2002). Those changes are often accompanied by changes of the texture of the oral mucosa.
Early detection of mouth cancer results in a 90% survival rate compared to 50% in late detection of mouth cancer.
According to the Oral Health Foundation’s State of Mouth Cancer UK Report 2020/2021: ‘Awareness of the major signs and symptoms for mouth cancer are as low as 23%’.
Mouth, head and neck cancer examination
The Mouth Cancer Foundation recommends dental professionals carry out a mouth, head and neck screening on every patient over the age of 16 at least once a year.
The authors describe a thorough systematic mouth, head and neck examination.
The examination requires:
- A pair of gloves
- Good lighting
- Gauze.
The screening is divided into two components: extraoral and intraoral.
Extraoral examination
The head and neck are visually inspected for any signs of asymmetry, scars or lumps or skin abnormalities. It is important to look, listen and feel every area that is being examined.
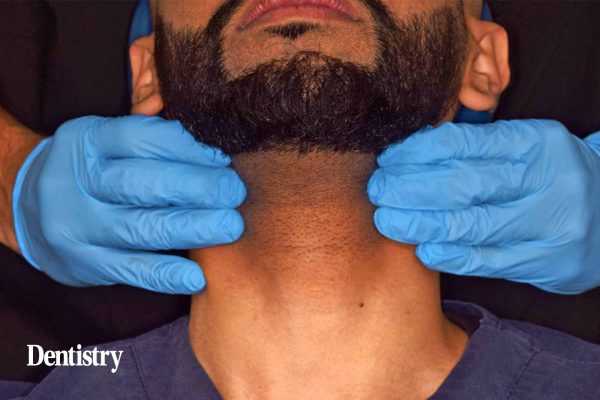
The neck examination can be conducted one side at the time or both sides contemporary.
A gentle pressure is applied by two finger tips to identify any asymmetry or indurated lump. It is generally started at the level of the submental nodes, moving to the submandibular then upper middle and lower cervical area.
Supra clavicular, posterior cervical and the parotid glands are also inspected and palpated. Those areas are also referred as levels I to VI (Figures 1-7).
Intraoral examination
All dentures should be removed before the examination.
The examination of the oral cavity can be conducted with the use of mirrors or clinician’s fingers as retractors. Fingers allow the clinician not only to visualise the oral mucosa but to also feel at the same time if there are any areas of induration within the soft tissue or changes of texture of the mucosa.
The lower lip is pulled downward and the upper lip upwards and manipulated with the thumb and index finger (Figures 8, 9 and 10).
The right and left buccal mucosa are pulled away, one side at a time, to allow the inspection of the retromolar area and the upper and lower vestibule (Figures 11 and 12).
Tongue inspection
The tongue is thoroughly inspected, as it is the most common area of mouth cancer presentation.
The use of a white gauze is extremely helpful as it allows clinicians to stretch the tongue to both sides to inspect lateral borders and ventral area of the tongue (Figures 13-17).
The floor of the mouth is another area of the oral cavity at high risk of cancer presentation. The index finger can be used to lift the side of the tongue and explore the mucolingual fold and floor of the mouth.
The bimanual palpation of the floor of the mouth can be done using one or two fingers of each hand trying to gently compress between them the floor of the mouth and the neck to look for lumps and fixed lesions.
Gingival tissues
Gingival tissues are generally inspected visually during the manipulation of the lips and inspection of the buccal mucosa.
The patient is then asked to lift the tip of the tongue to allow visual inspection of the ventral area of the tongue and the roof of the mouth (Figure 18).
With a gentle and firm pressure of one finger to the dorsum of the tongue, the patient is asked to say the vocal ‘ahhh’, the posterior wall of the oropharynx and the tonsillar area can be exposed for inspection (Figure 19).
The roof of the mouth is inspected directly by asking the patient to lift the chin up (Figure 20). Dental mirrors can be used to inspect areas of the oral cavity that are difficult to be examined directly like the lingual side of the lower jaw and the maxillary tuberosity.
A thorough systematic mouth, head and neck examination can be completed in less than five minutes.
The Mouth Cancer Foundation and Oral Health Foundation have videos that shows a mouth, head and neck examination taking place. We encourage you to watch these videos.
Risk factors
It is also vital that we inform our patients of the risk factors of mouth cancer, which include:
- Tobacco use
- Heavy alcohol use
- Excessive sun exposure to lips
- Human papillomavirus
- History of cancer
- Weakened immune system.
Suspicious areas
If any unusual findings are discovered during the examination, a review appointment should be made for two weeks after the initial examination.
The size, shape, colour, texture and the position of the suspicious areas should be recorded. It is also a good idea to take clinical photographs of the area of concern.
The oral mucosa generally heals itself in two weeks, if the suspicious areas are still present at the review appointment, the patient should be referred for further investigation.
Highly suspicious lesions (Figure 21) should be referred urgently under the two weeks wait referral pathway.
Self-examination
Mouth cancer self-examination is recommended by a number of organisations.
The Mouth Cancer Foundation launched Bite Back at Mouth Cancer, which is a head and neck cancer check that can be carried out by anyone, at any time.
The self-examination should be carried out by everyone over the age of 16 years, ideally once a month.
Dental professionals should encourage patients to visit www.mouthcancerfoundation.org/self-examination for a pictorial step-by-step guide and further details.
Mouth Cancer Action Month
To raise awareness, Mouth Cancer Action Month takes place each and every November. This initiative is supported by the Oral Health Foundation and the Mouth Cancer Foundation.
The campaign enables people to become ‘mouthaware’ and save lives through prevention and early detection.
There are numerous ways to get involved with Mouth Cancer Action Month. Some of the most popular include:
- The Blue Ribbon Appeal
- Arranging events to raise awareness of mouth cancer
- Taking part in the Mouth Cancer 10km Awareness Walk
- The Blue Lip Selfie campaign
- Donating to mouth cancer charities
- Encouraging mouth cancer self-examinations.
Conclusion
Our goal should be to detect mouth cancers before our patients present with symptoms.
Early detection and diagnosis of mouth cancer dramatically improves survival rates and also makes treatment and rehabilitation easier. Systematic and regular screenings save lives.
Taking part in Mouth Cancer Action Month is an excellent way to help raise awareness of this devastating condition.
We encourage you to get involved this November.
To find out more about Mouth Cancer Action Month, visit either the Mouth Cancer Foundation website (www.mouthcancerfoundation.org/mouth-cancer-action-month) or the Oral Health Foundation website (www.dentalhealth.org/mouthcancer).
Further reading
- Mignogna MD, Fedele S, Lo Russo L, Ruoppo E, Lo Muzio L (2002) Costs and effectiveness in the care of patients with oral and pharyngeal cancer: analysis of a paradox. Eur J Cancer Prev 11(3): 205-8
- Oral Health Foundation. The State of Mouth Cancer UK Report 2020/2021: www.dentalhealth.org/thestateofmouthcancer
- Oral Health Foundation. How to spot mouth cancer: www.dentalhealth.org/spotthesigns
- Mouth Cancer Foundation. Screening for head and neck cancer: www.mouthcancerfoundation.org/screening-by-a-dentist.