INTRODUCTION
Historically, everything from autogenous bone to xenografts, allografts, and alloplastic materials has been used and studied in dentistry when a graft or graft substitute is needed. These different materials have all been used with great success over the years, and they continue to provide clinically successful results. The alloplastic class over the years has become an exciting class since it is continually being advanced at a greater rate by new products than the allograft and xenograft classes.
Everyday, practitioners are faced with the need to graft and regenerate new bone. This can be an extraction site, an existing defect, or in combination procedures such as immediate implant placements or sinus elevations. The purpose of a graft material is to not only maintain clinical bone volume but also also to provide a framework for new bone growth as the particles are resorbed for new bone regeneration. Only in the case of an autograft will osteogenesis occur, as there are live cells capable of proliferating to create new bone. Therefore, a bone substitute is a natural or synthetic material, often containing only a mineralized bone matrix with no viable cells.1
In studies, the 3 main classes of graft materials (allograft, xenograft, and alloplast) all showed the presence of newly formed bone with residual graft particles and connective tissue in greater or lesser amounts. The presence of newly formed bone in direct contact with residual particles of each bone substitute material indicated the adequate osteoconductive capacity.2
This article will compare the makeup and advantages/disadvantages of the materials noted above and then focus on a material consisting of non-ceramic, synthetic, bioactive resorbable calcium apatite crystals known as OsteoGen (IMPLADENT LTD). These hydrophilic cluster particulates have physicochemical and crystallographic properties similar to human minerals. The low-temperature, bioactive calcium phosphate mineral also has the ability to control the migration of connective tissue.3
We are now going to look at and compare individual classes of graft materials to better understand the advantages of OsteoGen.
AUTOGENOUS BONE
Autografts remain the gold standard for grafting materials as they are still the only graft material that possesses the 4 fundamental biological properties required for bone regeneration, but they are not without issues.1,4
An advantage of the use of autogenous bone graft materials is that they represent the highest degree of biological safety, and there are no histocompatibility or immunogenicity issues associated with their use.
Even with autogenous bone grafts being considered the optimal choice for augmentation, the procedure usually requires harvesting bone from a distant donor site. This resulting second site morbidity can, has, and will continue to lead to patient dissatisfaction.
ALLOGRAFTS
Allograft materials, which are derived from cadaveric sources, have been used for decades with great success. These materials come in many forms, including mineralized and demineralized particulates and puttys. They are also available in cortical and cancellous formulations or a blend of the 2.
On their own, cancellous autografts and allografts have poor mechanical strength in addition to exhibiting inadequate healing capacity. The tissue-processing techniques, including treatment with alcohol, acetic acid, or nitric acid, reduce the materials’ osteoinductive capabilities.1,5 These graft materials can also cause local host inflammatory responses, which can result in fibrous tissue formation rather than healthy bone. This is of concern and can produce up to 62% connective tissue, which is not conducive to good implant support after load (Figure 1).
Figure 1. Four clinical studies of allografts (mineralized or demineralized) conducted at New York University College of Dentistry and the University of Texas San Antonio from 2002 to 2012.
Cortical particles, on the other hand, do provide structural support and provide a mineral storehouse, but these take longer to resorb. This increased resorption time is a distinct advantage when trying to either rebuild height/width or maintain osseous architecture when thin cortical plates are present after an extraction.
The downside, a common issue with all types of particulate grafts, is the possibility of migration or loss of material. Even if the particles are bound, as in bone putty by a binder, the addition of fluids, including blood, can wash these products out during clinical delivery. Finally, the literature supports the possibility of disease transmission by this class of products.6
Caution: Not all mineralized graft materials are the same.
ALLOPLASTS
Historically, many substances have been used as components for grafting in dentistry, either by themselves or as a binder with other graft materials. This author has used many of these with varying results. Calcium phosphate is one substance that has been used as a bone cement either to deliver antibiotics locally or to bind allograft or xenograft particulates. One example of this type of product is Fusion Bone Binder (Park Compounding Pharmacy). Bi-phasic calcium phosphate products such as Augma Biomaterials’ 3D Bond (Augma Biomaterials) and Bond Apetite are products that are used alone as a graft material. Beta-tricalcium phosphate (β-TCP) products such as Cerasorb M (Curesan) is another material used alone to graft sockets or defects around implants.
DENSE SINTERED ALLOPLASTS AND XENOGRAFTS
The Food and Drug Administration refers to dense, non-resorbing products as bone filler and augmentation materials (BFAM), and these have been used extensively for many years. To overcome potential immunogenicity and morbidity at donor sites, artificial synthetic bone substitutes and natural materials are manufactured to closely mimic the biological properties of natural bone.1 These alloplast materials are either derived from natural substances (ie, coralline) or man-made and can be a homogenous product or a mix of materials. A variety of synthetically and organically derived dense bone formulations have been used in dentistry and medicine. In dentistry, they are used for the therapeutic repair and restoration of osseous ridge defect sites, post-tooth extraction (including periodontal reconstruction), sinus augmentation with and without implants, and post cyst removal with questionable results. Since these products have weak regenerative abilities on their own, highly sintered alloplastic and organic bone substitutes are often augmented with growth factors and membranes at an increased cost to the practitioner.
When evaluating the rates of resorption of ceramic hydroxyapatite (HA) alloplastic materials, the results are questionable. Densely sintered at high temperatures, pure ceramic HA has low microporosity and high density and is prepared in relatively large particle size with long resorption times. Essentially, these materials closely resemble ceramics. Sintered (non-resorbable) HA materials,7 xenografts, and allografts are often subject to fibrous tissue encapsulation rather than becoming a viable part of the host bone.8
Upon tooth extraction, the goal is complete regeneration while preventing pathology from arising that could signal the patient’s immune response against getting involved, depending upon the type of graft material used. One consequence is the involvement of macrophage cells. In extraction sites where dense products such as ceramic HA, TCP, glass, polymers, coralline, and xenografts are placed, these macrophages are recruited. This is in contrast to the normal mechanism of osteoclastic breakdown.
These cells are signaled by an immune response to remove the graft material as foreign matter, and these 18-µm cells will continue to enter the socket area through the nutrient canals in the lamina dura (Figure 2).

Figure 2. The tooth-alveolous construct.
This immune response is inevitable in the use of these products, and the immune system’s mechanism is to eventually produce multi-nucleated giant cells to fragment (not phagocytose) these dense graft materials and transport the residual pieces to larger filters in the body (ie, lymph nodes, lungs, and the spleen), resulting in the patient’s compromised immune system.9,10
Studies have shown that highly dense bovine xenografts have also been shown to induce the formation of giant cells relatively early in the healing process.11
Compared with allogeneic and xenogenic bone grafts, common advantages of non-resorbable alloplastic bone substitutes are the standardized product quality and absence of infectious disease risk. The main advantages of alloplastic non-resorbing bone substitutes involve their biological stability and volume maintenance, which allow cell infiltration and remodeling.12 Originally HA ceramic and β-TCP products comprised 80% of all alloplastic bone graft products in the market.
Xenografts can be derived from sources including bovine and porcine origins, with bovine being the most prominent graft source in the industry. Xenografts carry with them the potential for immunologic reaction resulting in the patient mounting a host immune response against the grafting material. The long-term clinical use and safety of xenografts and their potential association with severe immune responses, as well as objections to their use for both religious and ethical reasons, are valid concerns.
Dental literature has rarely addressed the clinical risks and complications of anorganic bovine bone as a grafting material. However, the scarce literature on complications does not mean that such events are unusual. Often, the negative findings are not published or are not being submitted for publication in dentistry; ignoring the negative outcomes is worrisome as it skews the scientific literature. To the authors, a major concern was the late complications caused by product not resorbing, extending from 2 to 13 years after what was considered to be a successful treatment outcome. In the study, adverse effects presented in the case series report included sinus and maxillary bone pathoses, displacement of the graft materials, oroantral communications, implant failure, foreign body reactions, encapsulation, chronic inflammation, soft-tissue fenestrations, and associated cysts.13
Finally, the amount of time it takes for full “resorption” of the bovine xenograft material is a potential issue due to the fragmentation of the particulate by multi-nucleated giant cells, which is of immunologic concern. Human biopsies after sinus augmentation confirm that particles of bovine-derived bone substitutes can still be found up to 10 years postoperatively.14
RESORBABLE CALCIUM APATITE CRYSTALS AND CLUSTERS
OsteoGen has been used as a particulate graft material since 1984 and has documented clinical success for use with implants, general osseous repair,15 periodontal procedures,16 and sinus lifts.17 When first developed and brought to market, OsteoGen crystals and clusters were used either alone or mixed with other graft materials to extend the amount of graft and to enhance new bone growth. Over the years, product development to address the needs of practitioners has driven new products that contain the OsteoGen crystals mixed with highly purified Achilles tendon collagen. These products include OsteoGen Plugs, OsteoGen Strips, OsteoGen Blocks, and OsteoGen Plates (Figure 3).

Figure 3. Available OsteoGen (IMPLADENT LTD) products.
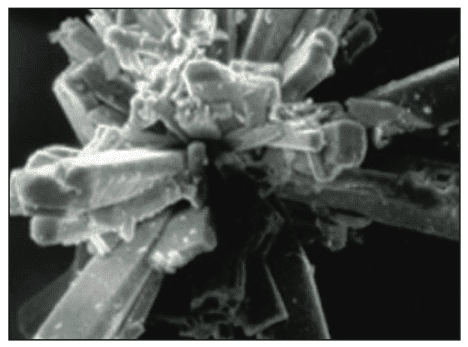
The bioactive crystal is grown utilizing a unique low-temperature production process that generates osteoconductive and resorbable low-density crystals and crystal clusters (Figure 4). It has a unique calcium-to-phosphate ratio similar to human bone that is neither a β-TCP nor a dense, non-resorbable ceramic HA.

Figure 4. Scanning electron micrograph of the OsteoGen crystal.

Figure 5. A 3-month histology by Dr. Kyle Hale at the University of Texas Health and Science Center.
As discussed previously, a non-autogenous bone graft material should ideally be non-antigenic, bioactive to control migration of connective tissue, osteoconductive, and synthetically derived with a clinically acceptable time frame of resorption of the majority of such material (Figure 5). The material does have physicochemical and crystallographic properties relatively similar to the host bone (Figure 6) and possesses a bioactive resorptive chemical potentiality to induce favorable cellular response for new bone formation by the action of ionization into calcium and phosphate ions in a chemotactic state.3 What this means is that the breakdown of the clusters produces the optimal environment on a cellular level for bone regeneration.

Figure 6. A fractured cross section of OsteoGen bioactive crystal with similarity to natural bone.
The clusters are a highly microporous, non-sintered, non-ceramic material composed of small and large crystals and hydrophilic clusters with a controlled, predictable rate of resorption based on the patient’s age and metabolism.
As opposed to particulate grafting materials on the market today, the plugs and strips prevent the migration of the OsteoGen crystals from the recipient’s surgical site by binding the crystals with collagen. With an approximate ratio of 60/40 mineral to collagen, it is similar to the makeup of native bone, and the distribution of OsteoGen crystals to porous collagen matrix creates an environment conducive to angiogenesis, cell proliferation, and new bone growth. The bioactive definition relates to the nature of the graft’s ability to form new bone by controlling migration of connective tissue and releasing calcium ions to stimulate new bone formation.
One of the main advantages of OsteoGen bioactive crystals is the ability to provide Ca+ ions directly into the site where bone growth and maturation will occur. When the composite is fully saturated with blood, these ions are released at an optimal level to facilitate healthy bone regeneration.
Local Ca+ levels in the grafted area control osteoblastic viability, proliferation, and differentiation and are concentration-dependent.
- Too high: >10mM results in apoptosis.
- Optimum: 6 to 8mM results in proliferation.
- Too low: 2 to 4mM results in proliferation and survival without differentiation.
Various clinical studies and recently published papers have confirmed OsteoGen’s bioactivity.
In a split-mouth study conducted by Yosouf et al,18 it was shown that, when compared to healing without a graft (control), ridge preservation was greatly enhanced by the use of an OsteoGen Plug. Results showed a 60% improvement when grafting with an OsteoGen Plug as 0.56 mm was lost vertically with the plug compared to 1.47 mm lost in the control. When looking at horizontal grafting, 0.9 mm was lost horizontally compared to 2.26 mm in the control. This minimal amount of bone loss is comparable to levels lost when utilizing an allograft and a membrane,19 although Yosouf et al18 achieved these results with the use of a Plug alone and no membrane.
Jones et al20 directly compared an OsteoGen Plug to a Collagen Xenograft Plug (Salvin Dental Specialties) and human bone allograft. It was found that osteoblast proliferation throughout the OsteoGen Plug was between 3 and 6 times greater compared to the xenograft plug or allograft. Additionally, live cell images showed significantly greater osteoblast activity at multiple time periods compared to the xenograft material, which could not sustain the cells. Also, this study showed significantly higher porosity levels (94.4%) for the OsteoGen Plug compared to xenograft material (75.2%) and allograft (55.8%). The study concluded that the OsteoGen Plug demonstrated significantly better biocompatibility compared to the xenograft option and the allograft option alone.
Jafarian21 compared the bone quality attained when using an OsteoGen Plug without a membrane to the bone quality attained using Biohorizons’ MinerOss corticocancellous allograft particulates and a dense PTFE membrane. The author concluded that there was no significant difference in bone quality measured by histomorphometry for placing an implant at 3 to 5 months between the OsteoGen Plug without a membrane and the current gold standard of corticocancellous allograft covered with a membrane.20
The following case series will reinforce the literature with regard to the uses and results of this alloplast plug.
RIDGE PRESERVATION
The most common observation of insufficient quantity of bone in dentistry is following tooth loss, where rapid resorption of alveolar bone occurs due to an absence of intraosseous stimulation that would typically occur via the periodontal ligament fibers.1,22,23 The amount of resorption is greatly dependent upon the reason for the extraction and the length of time pathology has been present. Studies and anecdotal clinical evidence provide the rationale for grafting fresh extraction sockets.
During the first year after tooth loss, a patient can see possibly 40% to 60% of the width and height of the alveolar ridge resorb after tooth extraction. Preserving the alveolar ridge offers patients choices in their restorative treatment plans, including endosseous implants.24
All successful ridge preservations have a common starting point, and that is the atraumatic extraction.25 There are a plethora of instruments available, and practitioners use just as many techniques to remove teeth. Though the specific techniques to achieve this will not be discussed in detail, the result by the use of any instrument or technique should minimize soft- and hard-tissue trauma.
SOCKET PRESERVATION CASE
The patient presented with a non-restorable maxillary right second molar (Figure 7a). Although the patient would likely not suffer any functional deficiency when chewing, he chose to have the site grafted in order to keep the possibilities open for an implant placement at a later date. After sectioning the roots for a less traumatic extraction (Figure 7b), the individual roots were removed while being careful not to damage the buccal plate (Figure 7c).

Figure 7. Socket preservation case.
Once the roots were removed, the sockets were thoroughly debrided to not only clean out any granulation tissue but also to produce copious bleeding. This bleeding is extremely important to kick off healing through what is known as the Regional Acceleratory Phenomenon by making holes through the lamina dura into cancellous bone and recruiting osteoclast cells. The OsteoGen Plug was then cut with scissors (Figure 7d) into a 3-root-like plug and placed into the socket (Figure 7e). The blood was allowed to soak into the plug by compacting the plug very gently into the socket to allow it to conform to the site (Figure 7f). A figure 8 chromic gut suture was utilized to hold the plug in place (Figure 7g). A primary closure or use of a membrane was not necessary. The compacted plug creates a bioactive-crystal, “wall-like” membrane to control the downward migration of connective tissue.
A radiograph taken immediately post-op showed that the plug itself was radiolucent (Figure 7h) and would become more radio-opaque as it was replaced by native bone. This unique aspect allows a practitioner to easily know when the site is ready for further treatment.
An intraoral photo of the site at one month demonstrates the complete closure of the site by secondary healing (Figure 7i). The 3.5-month radiograph is indicative of how the socket radio-opacity changes during healing by showing bony reconstruction of the socket (Figure 7j).
GRAFTING THE GAP WITH IMMEDIATE IMPLANT PLACEMENT
Much has been written regarding how to manage the “gap” that results when an implant is placed in an extraction socket. When a dental implant is placed into a fresh extraction socket, the space between the implant periphery and surrounding bone is called the “gap” or “jumping distance.” Bone filling in the gap between the implant and the peripheral bone is important for integration and long-term success. The buccal aspect of an implant is of great concern, especially in the aesthetic zone, because the buccal bony plate is usually thin, and its resorption can result in soft-tissue recession.17
The horizontal gap, if less than 2 mm, will likely fill in without any intervention by the practitioner. In fact, it has been shown that it is possible to have complete fill-in with a gap of up to 4.2 mm, but this is not predictable. Due to this unpredictability, grafting the gap is a belt-and-suspenders approach to assuring that both hard and soft tissue remain stable through the healing process and result in the optimal aesthetics when treatment is completed.26
In 2012, Chu et al27 showed that the most predictable hard- and soft-tissue changes and aesthetic results when immediately placing implants in a fresh extraction socket occurs when the gap between the implant and the alveolus is grafted.
IMMEDIATE PLACEMENT CASE
Presenting with a failing maxillary right central (Figure 8a), this patient opted for extraction and immediate placement of an implant. After an atraumatic extraction of the tooth (Figure 8b), the tooth was evaluated to determine the amount and position of graft material to be placed. By laying an osteotomy bur on the root, this calculation is very easy to perform (Figure 8c).

Figure 8. Immediate placement case.
The osteotomy was prepared following standard protocol to ensure proper prosthetic position, and the site was checked for any inadvertent perforation. A portion of an OsteoGen Strip was rehydrated with sterile saline in preparation for use. As opposed to the plug, which is delivered dry into an extraction socket, the OsteoGen Strip is rehydrated beforehand to enhance its moldability to fill the gap between the implant body and the alveolus (Figure 8d).
The position of the implant preparation had been distalized to take advantage of bone contact on the distal wall of the socket and to place the long axis of the implant in the correct prosthetic position for a central incisor with a midline diastema (Figure 8e). After placement of the strip, the implant was driven into place, causing the moldable strip to fill in any gaps (Figure 8f). Placing the strip first will be easier in these kinds of cases rather than trying to place it after the implant is in place. A check film was taken to verify the position (Figure 8g) and show the area of graft placement in the remaining socket. A 3-mm-tall healing abutment was placed, and the site was sutured with PGA sutures (Figure 8h). At the time of placement, the stability was not at a level that would have allowed for direct, immediate temporization.
After 3.5 months of healing, the healing abutment was removed (Figure 8i), a digital impression post was placed, and the site was scanned for the final restoration. A custom titanium abutment with a full zirconium restoration was chosen for the final restoration and delivered a few weeks later (Figure 8j). The soft-tissue quantity and quality was excellent, and the patient was pleased with the outcome.
SINUS ELEVATION
Everything from autogenous bone to allografts, xenografts, and alloplasts has been successfully used as graft material in the sinus. The osteoconductive activity of various bone substitutes has been assessed according to the quality and quantity of newly formed bone in the augmented areas.28,29
The successful use of OsteoGen crystals in sinus elevation has been well-established for more than 30 years. In 1991, Wagner30 showed the efficacy of this material in a 3.5-year follow-up study, and Manso and Wassal17 expanded on this work with a 10-year longitudinal study.The introduction of OsteoGen Plugs and Strips simplifies both vertical and lateral approach subantral lifts. The issues of material migration due to settling or loss due to the presence of a perforation have been mitigated due to the collagen makeup of the products.
The use of these products as a graft material is independent of the type of lift or technique used. Either plugs, strips, or malleable OsteoGen blocks can be used depending on the clinical situation. This author prefers to use plugs for vertical lifts and strips for lateral approach lifts.
SUBANTRAL AND LATERAL SINUS LIFTS
In this case, the sinus floor needed a sub-5-mm lift to accommodate the apex of the implant to be placed (Figure 9a). An osteotome was used to up-fracture the floor after creating an osteotomy approximately 1 mm short of the sinus floor. A regular-size OsteoGen Plug (Figure 9b) was cut to the appropriate dimension needed for the lift (Figure 9c) and placed into the osteotomy using an osteotome (Figure 9d). The resulting lift showed a smooth membrane without any indications of a tear (Figure 9e). With the use of these plugs, even if there was a small perforation or tear, the plug would allow for healing of the Schneiderian membrane without loss of the graft.
The Caldwell-Luc procedure, or lateral approach lift, is used when the clinical amount of crestal bone is less than 3 to 4 mm and placement of an implant would result in very little stability or exposure into the sinus cavity. The use of OsteoGen Strips rather than plugs to graft this type of case was decided upon in order to allow better conforming to the walls of the sinus cavity.

Figure 9. Sinus elevation cases.
In this case, the sinus had pneumatized after extraction of the maxillary right first molar (Figure 9f) and required a lift of approximately 10 mm to accommodate the length of the intended implant to be placed.
After a window was cut in the lateral wall of the sinus with a #2 round diamond (Figure 9g), the OsteoGen Strips were soaked in sterile saline (Figures 9h and 9i) to rehydrate them and make them malleable. Strips are first placed against the medial wall, then superiorly (Figure 9j), anteriorly, and posteriorly. This ensures that there will be grafting material 360° around the implant (Figures 9k and 9l) prior to placing additional strips laterally.
The final radiograph, taken 4 months later, indicated the growth of bone around the implant and the successful lift (Figure 9m).
CONCLUSION
Many times, it is a patient preference or refusal of a material that will guide a practitioner toward the type of grafting material he or she can use in a case. Studies have shown the highest rate of refusal was observed for allografts and xenografts. The grafts with the lowest rates of refusal were autologous grafts (3%) and dense alloplastics (2%).31
An advanced composite graft material such as OsteoGen, in all its prefabricated shapes and formulations, has the advantages of ease of use, cost-effectiveness, clinical ease of delivery, and adaptability to its intended site when compared to the other grafting particulate options on the market today. It is a viable and, in many circumstances, a better long-term option for grafting than traditionally used xenografts and allografts.
Currently, and in the future, combining this product with growth mediators such as PRF or other substances will open new chapters of outstanding clinical results. It is very likely that, in the future, the use of allografts and xenografts will likely diminish, and alloplastic bioactive materials, which have high quality, safety, and ease of clinical delivery, will be the regenerative materials of choice.
REFERENCES
- Zhao R, Yang R, Cooper PR, et al. Bone grafts and substitutes in dentistry: a review of current trends and developments. Molecules. 2021;26(10):3007. doi:10.3390/molecules26103007
- Nappe C, Rezuc A, Montecinos A, et al. Histological comparison of an allograft, a xenograft and alloplastic graft as bone substitute materials. J Osseointegration. 2016;8(2):20–6. doi:10.23805/jo.2016.08.02.02
- Valen M, Ganz SD. A synthetic bioactive resorbable graft for predictable implant reconstruction: part one. J Oral Implantol. 2002;28(4):167–77. doi:10.1563/1548-1336(2002)028<0167:ASBRGF>2.3.CO;2
- Misch CM. Autogenous bone: is it still the gold standard? Implant Dent. 2010;19(5):361. doi:10.1097/ID.0b013e3181f8115b
- Roberts TT, Rosenbaum AJ. Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012;8(4):114–24. doi:10.4161/org.23306
- Simonds RJ, Holmberg SD, Hurwitz RL, et al. Transmission of human immunodeficiency virus type 1 from a seronegative organ and tissue donor. N Engl J Med. 1992;326(11):726–32. doi:10.1056/NEJM199203123261102
- Linkow LI. Bone transplants using the symphysis, the iliac crest and synthetic bone materials. J Oral Implantol. 1983;11(2):211–47.
- Toloue SM, Chesnoiu-Matei I, Blanchard SB. A clinical and histomorphometric study of calcium sulfate compared with freeze-dried bone allograft for alveolar ridge preservation. J Periodontol. 2012;83(7):847–55. doi:10.1902/jop.2011.110470
- Ahmadzadeh K, Vanoppen M, Rose CD, et al. Multi-nucleated giant cells: current insights in phenotype, biological activities, and mechanism of formation. Front Cell Dev Biol. 2022;10:873226. doi:10.3389/fcell.2022.87322
- Miron RJ, Zohdi H, Fujioka-Kobayashi M, et al. Giant cells around bone biomaterials: Osteoclasts or multi-nucleated giant cells? Acta Biomater. 2016;46:15-28. doi:10.1016/j.actbio.2016.09.029
- Barbeck M, Udeabor SE, Lorenz J, et al. Induction of multi-nucleated giant cells in response to small-sized bovine bone substitute (Bio-Oss) results in an enhanced early implantation bed vascularization. Ann Maxillofac Surg. 2014;4(2):150–7. doi:10.4103/2231-0746.147106
- Fukuba S, Okada M, Nohara K, et al. Alloplastic bone substitutes for periodontal and bone regeneration in dentistry: current status and prospects. Materials (Basel). 2021;14(5):1096. doi:10.3390/ma14051096
- Rodriguez AE, Nowzari H. The long-term risks and complications of bovine-derived xenografts: A case series. J Indian Soc Periodontol. 2019;23(5):487–92. doi:10.4103/jisp.jisp_656_18
- Piattelli M, Favero GA, Scarano A, et al. Bone reactions to anorganic bovine bone (Bio-Oss) used in sinus augmentation procedures: a histologic long-term report of 20 cases in humans. Int J Oral Maxillofac Implants. 1999;14(6):835–40.
- Wagner JR. Clinical and histological case study using resorbable hydroxylapatite for the repair of osseous defects prior to endosseous implant surgery. J Oral Implantol. 1989;15(3):186–92.
- Epstein SR, Valen M. An alternative treatment for the periodontal infrabony defect: a synthetic bioactive resorbable composite graft. Dent Today. 2006;25(2):92–7.
- Manso MC, Wassal T. A 10-year longitudinal study of 160 implants simultaneously installed in severely atrophic posterior maxillas grafted with autogenous bone and a synthetic bioactive resorbable graft. Implant Dent. 2010;19(4):351–60. doi:10.1097/ID.0b013e3181e59d03
- Yosouf K, Heshmeh O, Darwich K. Alveolar ridge preservation utilizing composite (bioceramic/collagen) graft: A cone-beam computed tomography assessment in a randomized split-mouth controlled trial. J Biomed Eng. 2021;14(2):64-73. doi:10.4236/jbise.2021.142007
- Cheon GB, Kang KL, Yoo MK, et al. Alveolar ridge preservation using allografts and dense polytetrafluoroethylene membranes with open membrane technique in unhealthy extraction socket. J Oral Implantol. 2017;43(4):267–73. doi:10.1563/aaid-joi-D-17-00012
- Jones K, Williams C, Yuan T, et al. Comparative in vitro study of commercially available products for alveolar ridge preservation. J Periodontol. 2022;93(3):403–11. doi:10.1002/JPER.21-0087
- Kumar P, Vinitha B, Fathima G. Bone grafts in dentistry. J Pharm Bioallied Sci. 2013;5(Suppl 1):S125–7. doi:10.4103/0975-7406.113312
- Misch CE, Dietsh F. Bone-grafting materials in implant dentistry. Implant Dent. 1993;2(3):158–67. doi:10.1097/00008505-199309000-00003
- Murray VK. Anterior ridge preservation and augmentation using a synthetic osseous replacement graft. Compend Contin Educ Dent. 1998;19(1):69-74, 76–7.
- Schlesinger C. Ridge preservation technique: there’s more than one way to fill the hole! Dent Today. 2019;28(3)42-27.
- Schlesinger C. A novel approach to grafting around implants. Dent Today. 2017;26(12):50-54.
- Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524–32, 534.
- Berberi A, Nader N, Noujeim Z, et al. Horizontal and vertical reconstruction of the severely resorbed maxillary jaw using subantral augmentation and a novel tenting technique with bone from the lateral buccal wall. J Maxillofac Oral Surg. 2015;14(2):263–70. doi:10.1007/s12663-014-0635-7
- Artzi Z, Nemcovsky CE, Tal H, et al. Histopathological morphometric evaluation of 2 different hydroxyapatite-bone derivatives in sinus augmentation procedures: a comparative study in humans. J Periodontol. 2001;72(7):911–20. doi:10.1902/jop.2001.72.7.911
- Wagner JR. A 3 1/2-year clinical evaluation of resorbable hydroxylapatite OsteoGen (HA Resorb) used for sinus lift augmentations in conjunction with the insertion of endosseous implants. J Oral Implantol. 1991;17(2):152–64.
- Fernández RF, Bucchi C, Navarro P, Beltrán V, Borie E. Bone grafts utilized in dentistry: an analysis of patients’ preferences. BMC Med Ethics. 2015;16(1):71. doi:10.1186/s12910-015-0044-6
ABOUT THE AUTHOR
Dr. Schlesinger has been placing implants for the past 28 years, and as an educator for the past 19 years, he has taught doctors worldwide about dental surgical procedures. Along with running a busy private practice in Rio Rancho, NM, he maintains a clinical advisory role with numerous dental product manufacturers. He can be reached at cdschlesinger@gmail.com.
Adj. Prof. Valen is the founder and CEO of Impladent. He can be reached at maurice@impladentltd.com.
Disclosure: Dr. Schlesinger is a paid consultant for Impladent. Mr. Valen is a nonpaid consultant for Solmetex and CEO of Impladent.
WEBINAR
Dr. Schlesinger will present a FREE CE WEBINAR on Wednesday, July 10, 2024 expanding on this article’s topic.
CLICK HERE TO REGISTER NOW.