INTRODUCTION
“Conservative” and “Necessary”: A “Marriage of Philosophies”
It has been stated by Shavell that “occlusion and morphology are the common denominators of all dentistry.”1 A single tooth or restoration can have a profound effect on the function and comfort of a patient if it is not properly integrated into the patient’s natural occlusal function.
It is unfortunate that “modern” dentistry has such a “conformative” approach under the guise of being “conservative” or committing “over-treatment.” With the “tooth-at-a-time” or “if it’s not broke, don’t fix it” approach, are we really doing our best to help patients keep their teeth for the rest of their lives?
How many teeth, as Dr. Harold M. Shavell would say, “have been sacrificed on the altar of false conservatism?” These are questions we all wrestle with every day in private practice. One thing that is important to remember is that the muscles always win!
Without proper integration into a non-interfering occlusal scheme, the best restorative effort will ultimately fail, regardless of the material used.
The following is a case report that illustrates these premises while addressing the replacement of a single-tooth restorative failure.2,3
A CLASS IV COMPOSITE FAILURE: CASE HISTORY AND RESTORATIVE PLAN
The patient in Figure 1 presented with a broken Class IV mesial incisal composite restoration on tooth No. 8. It had been replaced 3 times during the past year and had broken again. Aside from the amount of composite on the facial surface that extended beyond the fractured area, a majority of the lingual (palatal) surface of the tooth was worn through to the dentin due to hyperfunction in protrusive and lateral excursions for many years, creating a functional and an aesthetic dilemma for this patient.
A “conservative” approach may have been to simply bond the tooth again with composite and hope for the best. However, when considering the functional stress in this area, even with the best tooth alignment, this may not have been the best long-term approach. After all, how “conservative” is it to continually “assault” the tooth with rotary instrumentation to keep “fixing” a composite that continues to break? What about the alignment of the opposing teeth?
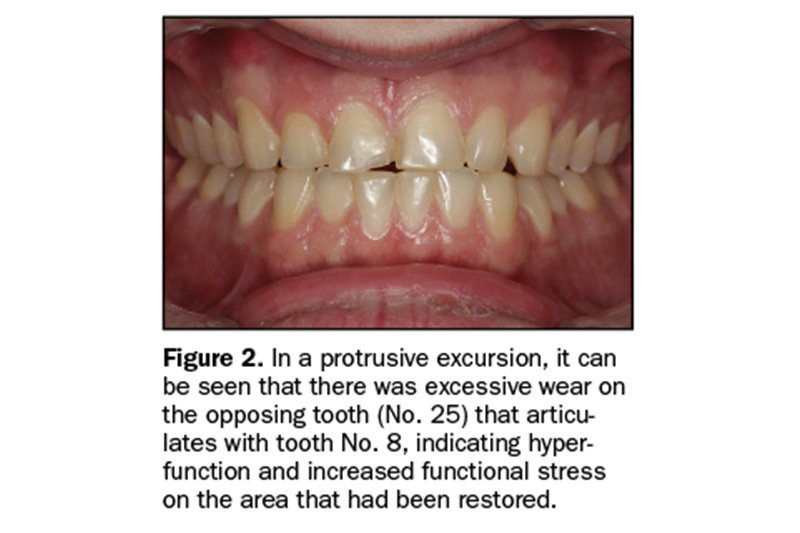
It can be seen in Figure 2 that excessive incisal wear was present on the incisal edges of teeth Nos. 24 and 25. From the incisal view (Figure 3), extensive wear is seen on all mandibular anterior incisal edges as a result of occlusion (occlusal disease) that is often seen yet left untreated.
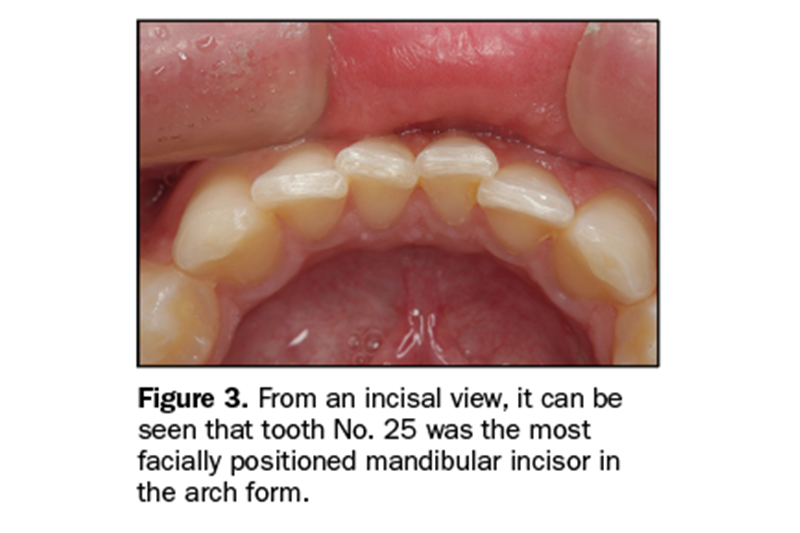
Tooth No. 25 was also facially positioned so that, in protrusive excursions, it engaged the palatal surface of tooth No. 8, prematurely placing additional stress on both the palatal surface and incisal edge of tooth No. 8 before coupling with the remainder of the maxillary anterior segment.
So, to address these issues restoratively, it involved more than just fixing a chipped composite restoration. Orthodontics to correct tooth alignment was discussed with the patient, but there was no interest. That being said, a “Plan B” could have been to restore tooth No. 25 in such a way that the position of the tooth facially and the incisal edge would not engage the palatal surface of tooth No. 8 prematurely, followed by restoring the palatal surface and incisal facial fractured area with ceramic to replace the lost enamel and reinforce what remained.
The decision was made to restore tooth No. 8 with a ceramic restoration and tooth No. 25 with a direct composite. Aesthetically, for tooth No. 8, an aesthetic match to tooth No. 9 could have been better achieved with layered ceramic.
Composite resin was chosen as a more conservative and less costly option for tooth No. 25, but the patient was told that it may require a ceramic restoration at a later time.
Operative Procedure No. 1: Tooth No. 25 Direct Composite Veneer
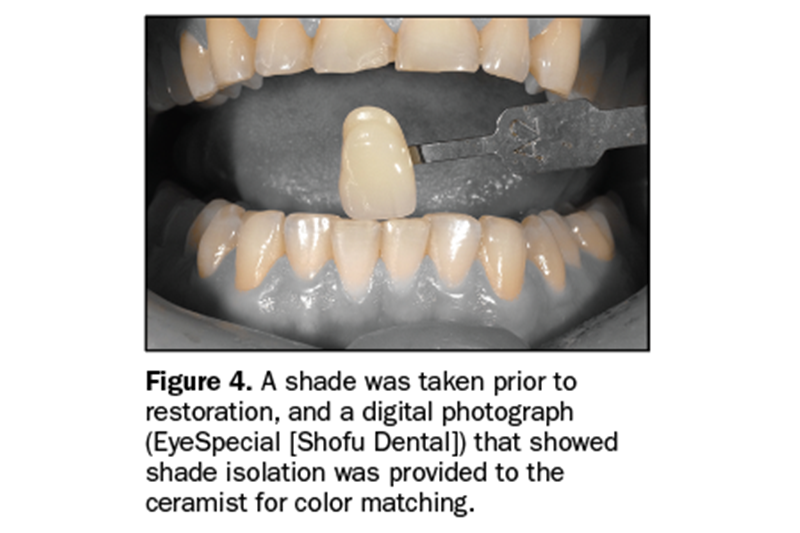
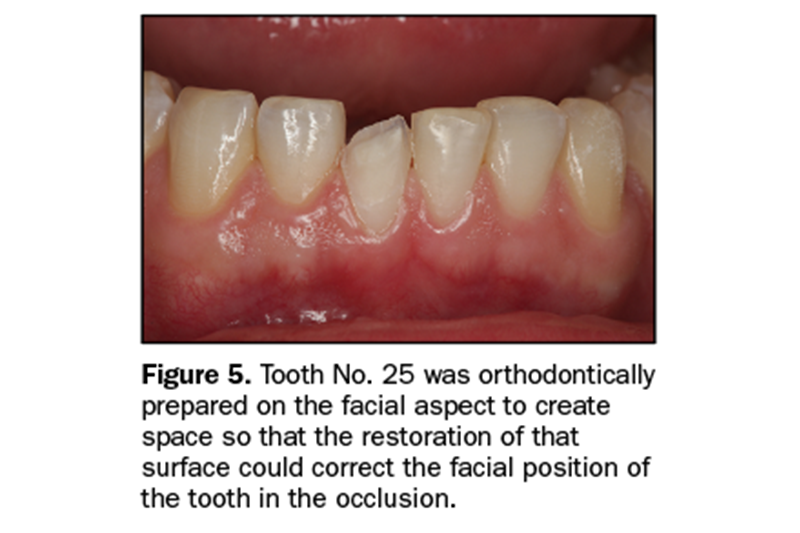
A preoperative shade was chosen and photographed (Figure 4) for the ceramist using a digital camera with a function that isolates the tooth shade from the rest of the oral cavity (EyeSpecial [Shofu Dental]). Next, the facial surface of tooth No. 25 was prepared orthodontically to move the facial surface and incisal edge lingually (Figure 5). It is important to note that the beveled facial surface of tooth No. 25 after preparation had a knife-edge cervical margin that was about 2 mm supragingival.
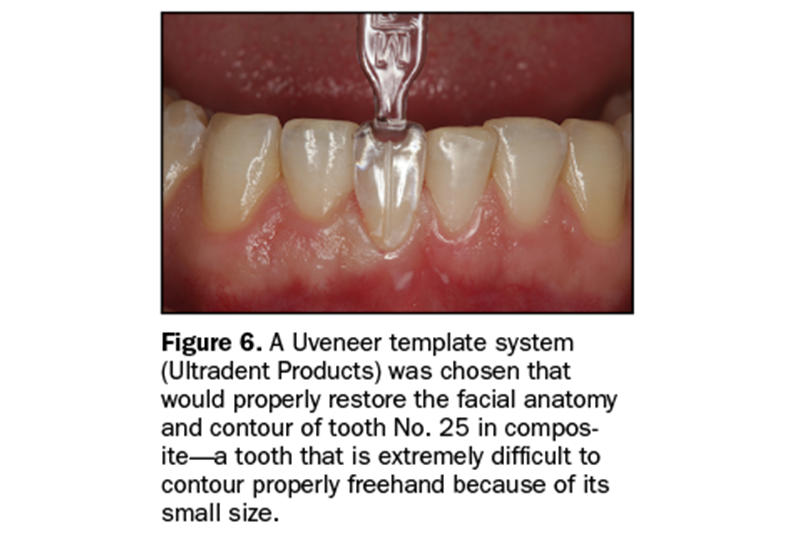
This “long bevel” allowed for a more aesthetic blend of composite and tooth structure while leaving the emergence profile of the natural tooth untouched. Figure 6 shows the positioning of a Uveneer template system (Ultradent Products), which was used to fabricate the facial and incisal anatomy in composite and “move” the tooth (tip) in the lingual direction. Prior to the placement of composite, the tooth (enamel) surface was etched with phosphoric etch (Ultra-Etch [Ultradent Products]) for 15 seconds, thoroughly rinsed, and then air dried.
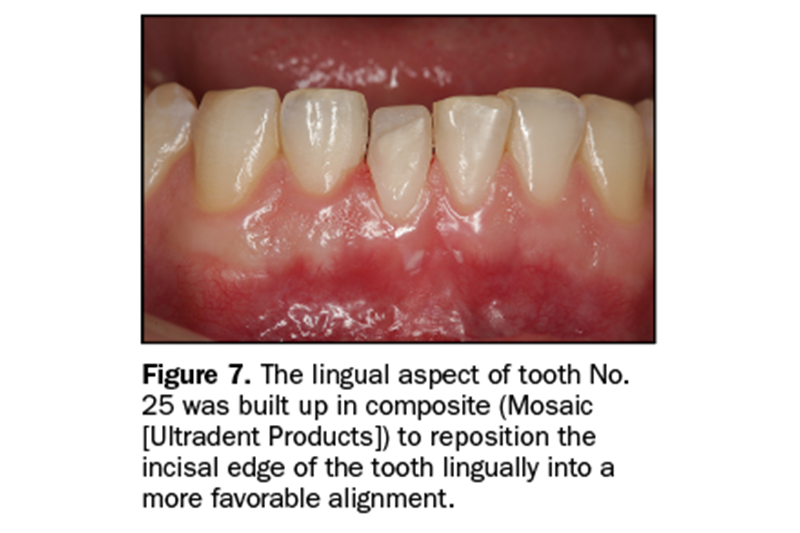
A universal bonding resin (Peak Universal Bond [Ultradent Products]) was applied to the tooth surface; air-thinned, evaporating the solvent; and then light cured for 20 seconds (VALO Grand [Ultradent Products]). Figure 7 shows the initial increment of composite used to build up the incisal one third of the tooth to its new “lingualized position.”
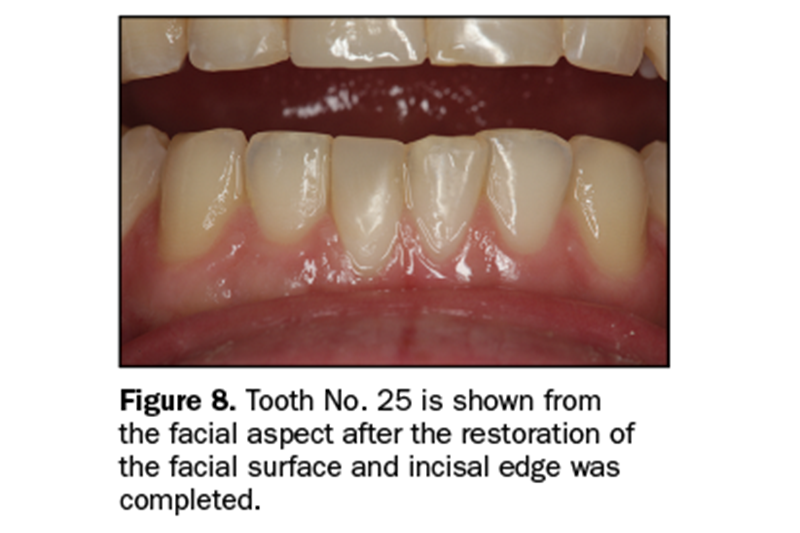
The Uveneer template system was then filled with the chosen shade of composite (Mosaic Universal Composite [Ultradent Products]) and placed on the facial surface of the tooth in the proper alignment with the adjacent teeth and light cured. Figure 8 shows tooth No. 25 after removal of the Uveneer template and some minor incisal adjustments and polishing.
Operative Procedure No. 2: Tooth No. 8 All-Ceramic Restoration
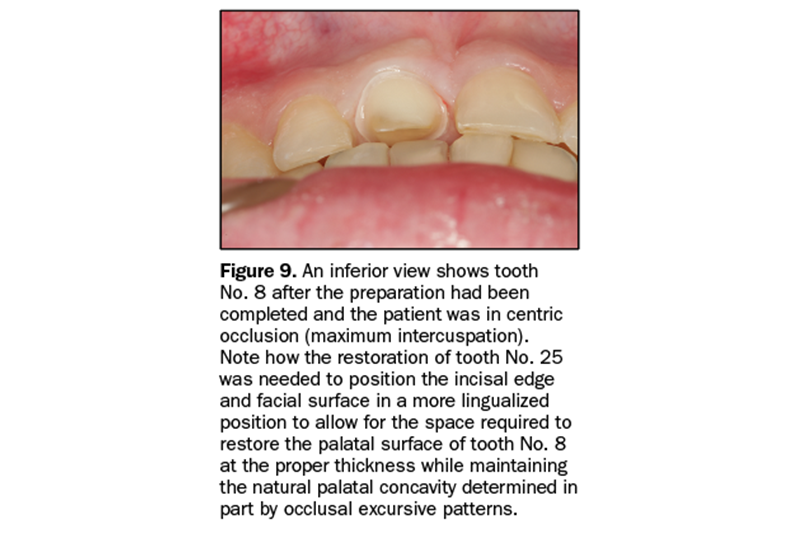
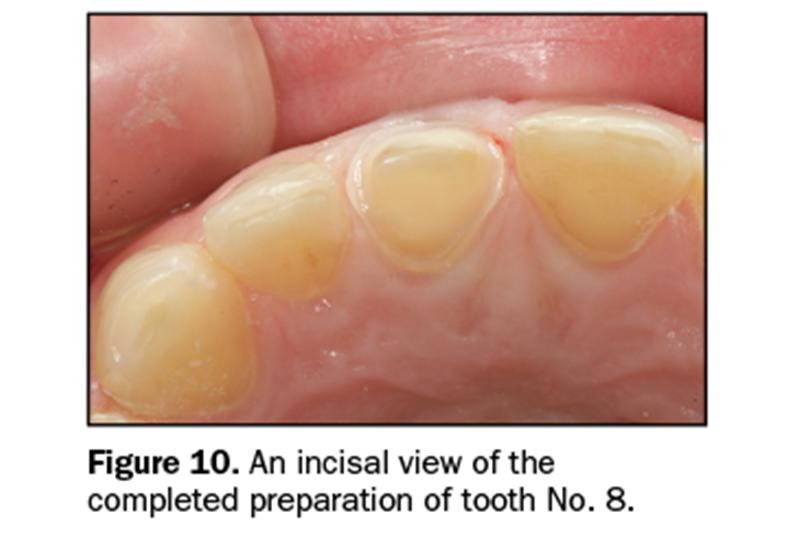
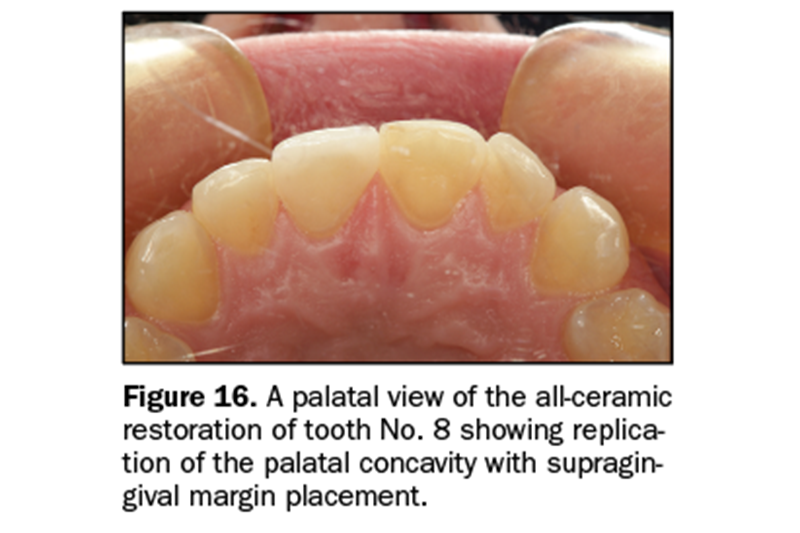
Tooth No. 8 was prepared for an all-ceramic crown. It is important to stress that the preparation of the palatal surface is critical. It must be prepared to 1.0 to 1.5 mm of reduction following the curvature of the unprepared palatal surface (maxillary palatal concavity).
This is so the restoration can follow the natural palatal curvature at the appropriate thickness of restorative material for strength. Remember, the maxillary palatal concavity is determined by the angle of the eminence and the envelope of function, both occlusal determinants that must be followed when restoring maxillary anterior teeth (Figures 9 and 10).
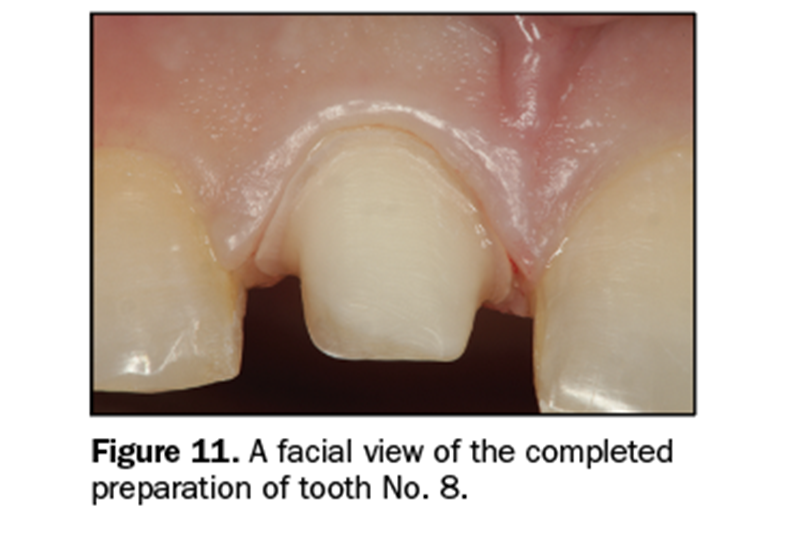
Once the preparation is completed (Figure 11), the master impression can be made.
The “2-Cord” Technique for Indirect Impression Making
A 2-cord impression technique is an extremely predictable way to capture quality master impressions for full coverage (circumcoronal) and partial coverage restorations with either intracrevicular or equicrevicular margins (at the free gingival margin).4 First, a #00 retraction cord (Ultrapak [Ultradent Products]) is placed at the base of the gingival sulcus around each preparation, starting from the lingual aspect, around the proximal to the facial aspect, then back through the opposite proximal area to the lingual starting point.
The excess at both lingual ends is trimmed, and the opposing ends of the cord are tucked into the lingual gingival sulcus so that they butt against one another (not overlapping). Once the first retraction cord is properly placed, and prior to placement of the second retraction cord, any minor marginal correction can be done to the preparation using a course or fine diamond instrument of the appropriate diameter. Next, a #1 cord (Ultrapak) is placed on top of the #00 in the same manner as previously described.
If desired, all cords may be soaked in a hemostatic solution (ViscoStat Clear [Ultradent Products]), and then the excess is removed with a 2 × 2 in gauze sponge prior to placement. Next, using a cotton pledget, the preparation is wiped with Consepsis (Ultradent Products) to make sure the surface is clean and free of “prep debris” from the diamond instrument.
When ready (usually after all cords are in place and the fit of the impression tray has been verified), the #1 cord is partially pulled out of the sulcus using an explorer on the facial aspect of each preparation, and the amount of retraction (and lack of moisture or blood contamination) is evaluated. Remember, the master impression must capture not only the entire restorative margin, but also 0.5 mm of the tooth/root surface apical to the margin.
If the marginal gingiva adjacent to any restorative margin rebounds to contact the tooth/margin after the top cord is pulled, a small piece of a larger diameter cord (#2) (Ultrapak) is placed into the affected area for an additional minute and then removed. This added retraction should be sufficient to create a space between the tooth surface and the inner dimension of the gingival sulcus. The goal of retraction is to “create a moat (a space in which to inject light-bodied impression material) around the castle (tooth preparation).”
A Super Pulsed Diode Laser as an Adjunct to Cord Packing
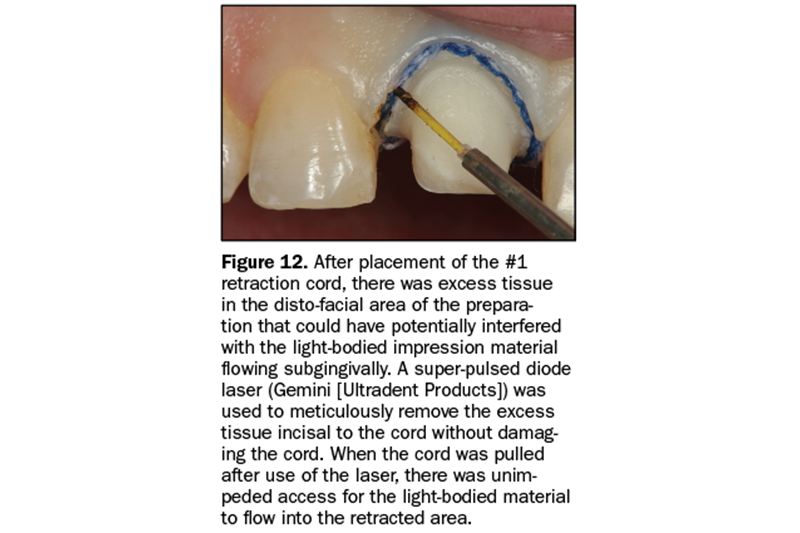
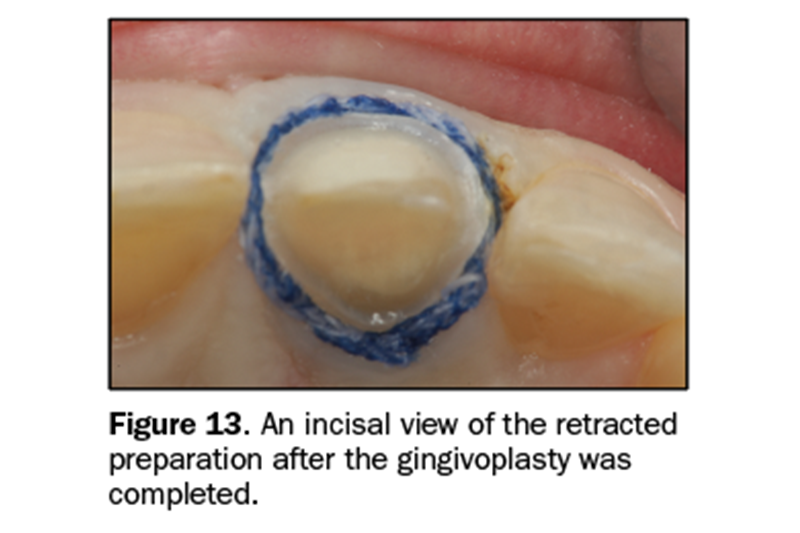
If any portion of the circumferential gingival tissue is not sufficiently retracted away from the emergence profile of the tooth/preparation after placement of the #1 retraction cord, a diode laser can be used to perform a minor gingivoplasty on the overlapping gingival tissue above the top cord so that it is visible prior to its removal. This is common in interproximal areas where the gingival tissues (papilla) may be slightly enlarged.
It is not recommended to hope that the heavy-bodied tray material will “push” the tissue out of the way to let the light-body material access the gingival crevice. Figures 12 and 13 show the super pulsed diode laser (Gemini [Ultradent Products]) performing a gingivoplasty above the top cord with the retraction cord entirely visible prior to its removal and injection of the light-body impression material. When the cord is removed, an impression of the margin and 0.5 mm of tooth/root surface apical to the margin is virtually assured.
To capture a precise master impression, light-bodied impression material should be injected not only around the prepared teeth but also over all occlusal and incisal surfaces so that the stone models can be accurately articulated. After injection of the light-bodied material, the impression tray with the heavy-bodied impression material is placed in the mouth for the appropriate time, based on the manufacturer’s recommendations.
Delivery of the All-Ceramic Restoration
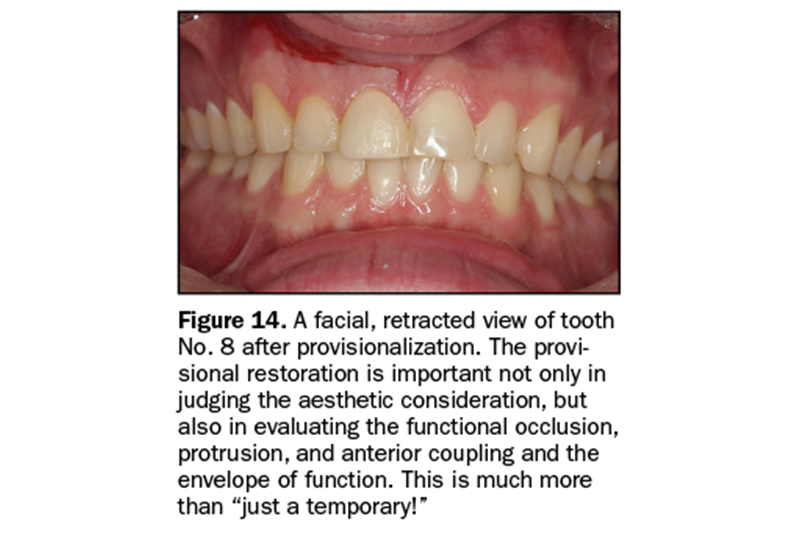
Figure 14 shows a retracted smile view of the provisional restoration and gingival tissues around tooth No. 8 prior to delivery of the definitive restoration.
After removal of the provisional restoration and any remaining provisional cement, the restoration was tried in, and the proximal contacts and occlusion were adjusted and then polished as necessary. Next, the preparation was disinfected with Consepsis. Also, the restoration had been etched by the laboratory, so the etched surface was treated with a silane coupler prior to cementation as per the manufacturer’s instructions.
The restoration was then luted using a dual-cured resin cement (PermaFlo DC Translucent [Ultradent Products]).
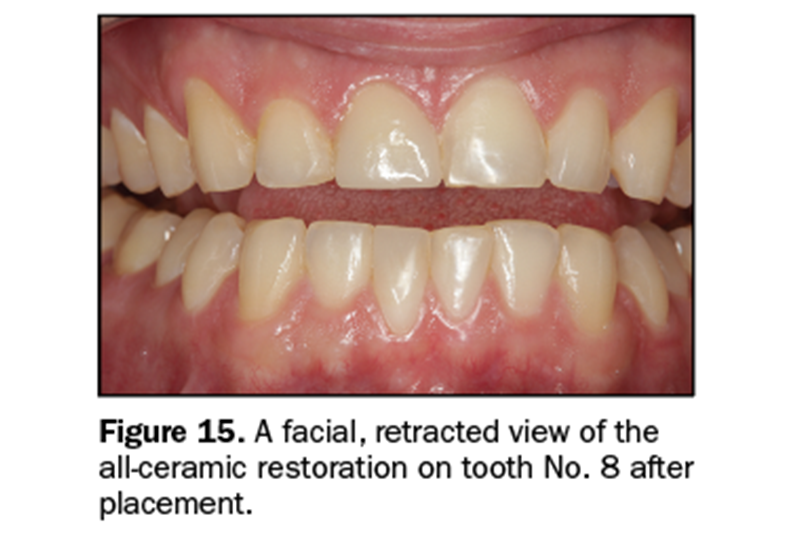
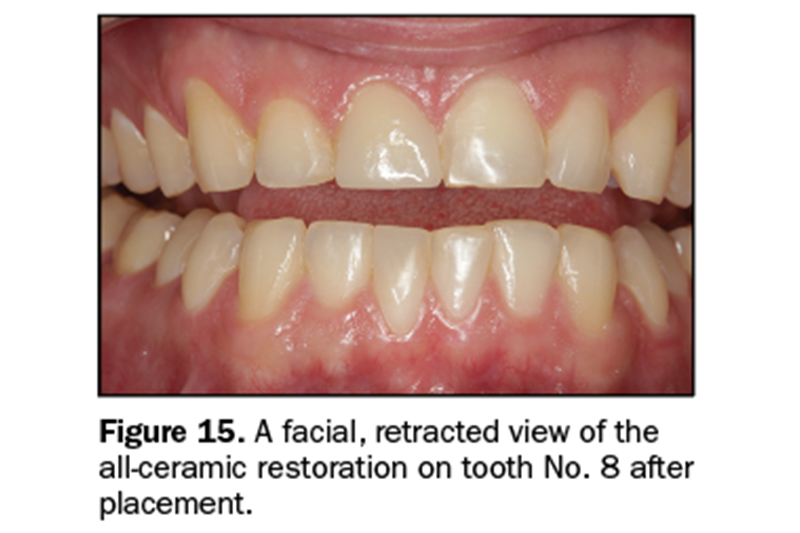
Figures 15 and 16 show the restoration of tooth No. 8 with an all-ceramic crown after cementation.
CONCLUSION
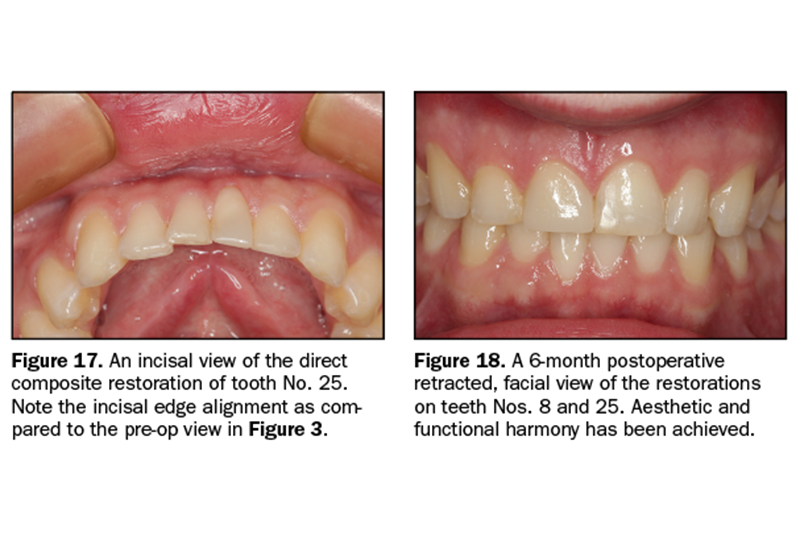
It is important to always consider that the restoration of a single tooth can affect the occlusion in a profound way. The reverse is also true: Not considering the occlusion can affect a single restoration both in contour and longevity. It is always recommended to consider these issues prior to any restorative endeavor (Figures 17 and 18).
REFERENCES
1. Shavell HM. Occlusion: lost art, lost discipline: Part 1. Journal of the Pakistan Dental Association. 2013;22:164-177.
2. Parker MW. The significance of occlusion in restorative dentistry. Dent Clin North Am. 1993;37:341-351.
3. Neff P. Trauma from occlusion. Restorative concerns. Dent Clin North Am. 1995;39:335-354.
4. Cloyd S, Puri S. Using the double-cord packing technique of tissue retraction for making crown impressions. Dent Today. 1999;18:54-59.
ABOUT THE AUTHOR
Dr. Lowe received his DDS degree from the Loyola University School of Dentistry in 1982. He is an assistant professor in the Department of Oral Rehabilitation Division of Restorative Dentistry at the James B. Edwards College of Dental Medicine at the Medical University of South Carolina. He previously taught at the Loyola University School of Dentistry while building a private practice in Chicago. Dr. Lowe currently maintains a practice in Charlotte, NC. He can be reached at boblowedds@aol.com.
Disclosure: Dr. Lowe received an honorarium from Ultradent Products.