The estimated lifetime probability of acquiring human papillomavirus in the United States.
Sex Transm Dis. 2014; 41: 660-664
Genital HPV Infection-CDC Fact Sheet.
Worldwide burden of cancer attributable to HPV by site, country and HPV type.
Int J Cancer. 2017; 141: 664-670https://doi.org/10.1002/ijc.30716
Human papillomavirus-associated cancers: United States, 2008-2012.
MMWR Morb Mortal Wkly Rep. 2016; 65: 661-666https://doi.org/10.15585/mmwr.mm6526a1
HPV-associated head and neck cancer: a virus-related cancer epidemic.
Lancet Oncol. 2010; 11: 781-789https://doi.org/10.1016/S1470-2045(10)70017-6
Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States.
J Clin Oncol. 2008; 26: 612-619
US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines.
J Natl Cancer Inst. 2015; 107: djv086
Human papillomavirus and rising oropharyngeal cancer incidence in the United States.
J Clin Oncol. 2011; 29: 4294-4301
Prevalence of oral HPV infection in the United States, 2009-2010.
JAMA. 2012; 307: 693-703https://doi.org/10.1001/jama.2012.101
Epidemiological trends of head and neck cancer in the United States: a SEER population study.
J Oral Maxillofac Surg. 2017; 75: 2562-2572
Trends in human papillomavirus-associated cancers: United States, 1999-2015.
MMWR Morb Mortal Wkly Rep. 2018; 67: 918-924https://doi.org/10.15585/mmwr.mm6733a2
HPV and cancer: how many cancers are linked with HPV each year? Centers for Disease Control and Prevention. 2022..
Table 78: Dental Visits in the Past Year, by Selected Characteristics—United States, Selected Years 1997-2017. Centers for Disease Control and Prevention. 2022..
Dental care utilization among the U.S. population, by race and ethnicity. American Dental Association Health Policy Institute. 2022..
Impact of a dental/dental hygiene tobacco-use cessation curriculum on practice.
J Dent Educ. 2002; 66: 1074-1078https://doi.org/10.1002/j.0022-0337.2002.66.9.tb03576.x
Using the hygiene visit to deliver a tobacco cessation program: results of a randomized clinical trial.
JADA. 1998; 129: 993-999https://doi.org/10.14219/jada.archive.1998.0353
Including vaccinations in the scope of dental practice: the time has come.
JADA. 2021; 152: 184-186
HPV Vaccination and the risk of invasive cervical cancer.
N Engl J Med. 2020; 383: 1340-1348
Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis.
Lancet. 2019; 394: 497-509
Healthy People 2030: increase the proportion of adolescents who get recommended doses of the HPV vaccine—IID-08. Office of Disease Prevention and Health Promotion, US Department of Health and Human Services. 2022..
National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years: United States, 2019.
MMWR Morb Mortal Wkly Rep. 2020; 69: 1109-1116
Getting human papillomavirus vaccination back on track: protecting our national investment in human papillomavirus vaccination in the COVID-19 era.
J Adolesc Health. 2020; 67: 633-634
Parent-reported reasons for nonreceipt of recommended adolescent vaccinations, national immunization survey: teen, 2009.
Clin Pediatr (Phila). 2011; 50: 1116-1124https://doi.org/10.1177/0009922811415104
Missed opportunities for HPV vaccination in adolescent girls: a qualitative study.
Pediatrics. 2014; 134: e666-e674
ADA adopts policy supporting HPV vaccine.
ADA News. November 5, 2018;
Policy on human papilloma virus vaccinations. In: The Reference Manual of Pediatric Dentistry. Revised 2020.
Oregon passes bill allowing dentists to administer vaccines.
ADA News. May 6, 2019;
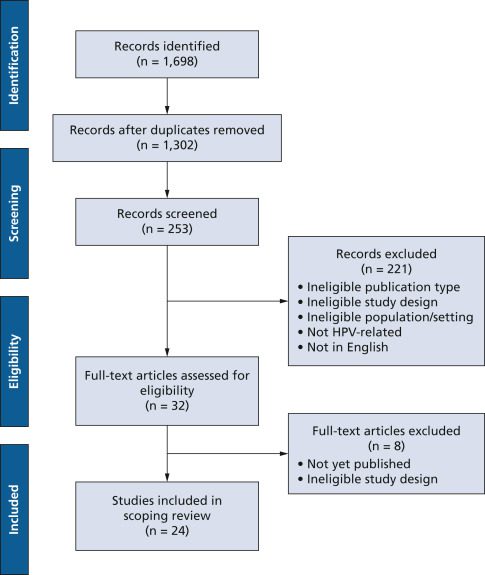
Scoping studies: towards a methodological framework.
Int J Soc Res Methodol. 2005; 8: 19-32https://doi.org/10.1080/1364557032000119616
Scoping studies: advancing the methodology.
Implement Sci. 2010; 5: 69https://doi.org/10.1186/1748-5908-5-69
Guidance for conducting systematic scoping reviews.
Int J Evid Based Healthc. 2015; 13: 141-146
Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework.
BMC Med Res Methodol. 2013; 13: 1-9https://doi.org/10.1186/1471-2288-13-48
Chapter 11: Scoping reviews.
in: Aromataris E. Munn Z. JBI Manual for Evidence Synthesis. JBI,
2020
PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation.
Ann Intern Med. 2018; 169: 467-473https://doi.org/10.7326/M18-0850
Rayyan: a web and mobile app for systematic reviews.
Syst Rev. 2016; 5: 210https://doi.org/10.1186/s13643-016-0384-4
Educational interventions on human papillomavirus for oral health providers.
J Cancer Educ. 2020; 35: 689-695https://doi.org/10.1007/s13187-019-01512-7
An educational intervention on HPV knowledge and comfortability discussing vaccination among oral health care professionals of the American Indian and Alaskan Native population.
Hum Vaccin Immunother. 2020; 16: 3131-3137
Assessing dentists’ human papillomavirus-related health literacy for oropharyngeal cancer prevention.
JADA. 2018; 149: 9-17https://doi.org/10.1016/j.adaj.2017.08.021
Dental professionals’ knowledge, attitudes, and practice behaviors related to human papillomavirus vaccination.
J Public Health Dent. 2020; 80: 61-69
Knowledge assessment of the dental community in Texas on the role of human papilloma virus in oropharyngeal cancer.
Tex Dent J. 2015; 132: 528-536
A multi-state evaluation of oral health students’ knowledge of human papillomavirus-related oropharyngeal cancer and HPV vaccination.
J Cancer Educ. 2020; 35: 1017-1025https://doi.org/10.1007/s13187-019-01561-y
HPV-related knowledge among dentists and dental hygienists.
J Cancer Educ. 2018; 33: 901-906https://doi.org/10.1007/s13187-016-1156-5
Health literacy approaches to improving communication between dental hygienists and patients for HPV-related oral cancer prevention.
J Dent Hyg. 2017; 91: 37-45
The effect of continuing education on dental hygienists’ knowledge, attitudes, and practices regarding human papillomavirus related oropharyngeal cancer.
J Dent Hyg. 2020; 94: 16-29
Exploring awareness, attitudes, and perceived role among oral health providers regarding HPV-related oral cancers.
J Public Health Dent. 2011; 71: 136-142
Impact of HPV immunization training on dental hygiene students’ attitudes and confidence regarding HPV preventive education.
J Dent Educ. 2020; 84: 88-93https://doi.org/10.21815/JDE.019.164
HPV vaccination and the role of the pediatric dentist: survey of graduate program directors.
Pediatr Dent. 2017; 39: 383-389
Knowledge of human papillomavirus among dental providers: a mixed methods study.
Vaccine. 2020; 38: 423-426https://doi.org/10.1016/j.vaccine.2019.10.068
Knowledge, attitudes and practices regarding human papilloma virus communication and vaccine advocacy among Minnesota dentists and dental hygienists.
J Dent Hyg. 2019; 93: 33-43
Dental provider practices and perceptions regarding adolescent vaccination.
J Public Health Dent. 2018; 78: 159-164
The role of the dental community in oropharyngeal cancer prevention through HPV vaccine advocacy.
J Cancer Educ. 2021; 36: 299-304https://doi.org/10.1007/s13187-019-01628-w
The role of dental providers in preventing HPV-related diseases: a systems perspective.
J Dent Educ. 2019; 83: 161-172
Dental opinion leaders’ perspectives on barriers and facilitators to HPV-related prevention.
Hum Vaccin Immunother. 2019; 15: 1856-1862https://doi.org/10.1080/21645515.2019.1565261
Evaluating the effectiveness of human papillomavirus educational intervention among oral health professionals.
J Cancer Educ. 2019; 34: 890-896https://doi.org/10.1007/s13187-018-1391-z
US oral health students’ willingness to train and administer the HPV vaccine in dental practices.
Prev Med Rep. 2019; 15100957https://doi.org/10.1016/j.pmedr.2019.100957
Are dental providers the next line of HPV-related prevention? Providers’ perceived role and needs.
Papillomavirus Res. 2018; 5: 104-108
An American Dental Association Clinical Evaluators Panel survey.
JADA. 2020; 151: 303-304.e2
The perspectives, barriers, and willingness of Utah dentists to engage in human papillomavirus (HPV) vaccine practices.
Hum Vaccin Immunother. 2019; 16: 436-444https://doi.org/10.1080/21645515.2019.1649550
Prevention of HPV-related oral cancer: assessing dentists’ readiness.
Public Health. 2014; 128: 231-238https://doi.org/10.1016/j.puhe.2013.12.002