INTRODUCTION
Dental implants have long been used to replace missing single teeth, multiple teeth, and full arches. The success rate of dental implants can approach 94.6% at 10 years.1 The failure of dental implants can occur for a variety of reasons, leading to the explanation of the failed implant fixture. Although residual excess cement from luting or bonding implant crowns to the stock or custom abutment intraorally is a common complication, the technique is still widely used.2-7 In 2018, Goodacre et al8 said that the most common complication reported with single implant crowns was abutment screw loosening. This screw loosening occurs on 4% of screw-retained crown-abutment complexes and 3% of cement-retained implant crowns. However, this is a vast improvement over previous abutment screw loosening data from 2003 of 25% with early screw designs.9
When the clinician or the patient discovers the crown-abutment complex is loose, it is critical to remove it immediately. Failure to do so will result in damage to the abutment screw, the abutment hexagon, or the dental implant. Fabrication of a new crown-abutment complex is relatively easy but adds cost for the patient. Conversely, if the loose crown-abutment complex is ignored, damage can occur to the dental implant. This damage may require an explanation of the implant fixture, adding potential morbidity and significant cost to the patient.
This technique article outlines the steps to remove, evaluate, and recommission the crown-abutment complex when the implant screw loosens, thereby lacking the appropriate torque to clamp the crown-abutment complex securely to the implant. Critical to the successful removal of a cement-retained crown is proper instrumentation. Dental burs specifically designed for ceramics are an absolute must to minimize the potential for chipping, fracture, or introducing microcracks in the ceramic layer that will later exhibit catastrophic failure. Komet USA manufactures burs specifically designed to grind ceramics, including zirconia (ZR6801 018). These feature a “white stripe” along with another colored stripe to indicate whether the bur is coarse (151-µm “green stripe”), medium (80-µm “blue stripe”), or fine (46-µm “red stripe”). Komet USA also manufactures metal-cutting burs, such as the H34 012 and H34L 012, which work extremely efficiently to penetrate metal crowns or cut metal crowns off. With our Tucker gold castings,10,11 we use the H34L 012 to smooth the sprue bump efficiently during laboratory fabrication.
Another point that needs to be emphasized is the need for dental handpieces that rotate true; eliminate bur chatter; and have good torque, adequate illumination, and good air/water spray to keep the field cool and clean.12 The Swiss-manufactured EVO.15 Micro-series CoolTouch+ electric handpieces (Bien-Air Dental) meet this criterion with extreme precision of rpm and torque by utilizing an iPod controller. The PM 1:1 straight nose cone (Bien-Air Dental) is excellent for making chairside adjustments to lithium disilicate (IPS e.max [Ivoclar]) or zirconia crowns using Komet USA’s yellow DCB diamond abrasives, ZR Flash polishers, and the “Footsie” polisher shape (94019C and 94019F).
The technique to recommission the crown-abutment complex is essentially an endodontic access, and the burs and handpieces utilized would be the same for creating access through a ceramic or porcelain-fused-to-metal crown. Essentially, when we are finished, we have turned a cement-retained implant crown into a screw-retained crown-abutment complex often referred to as a “screwmentable” or, as described by McGlumphy et al13 in 1992, “a combination implant crown.”
The technique for recommissioning a cement-retained crown with a loose abutment screw is as follows:
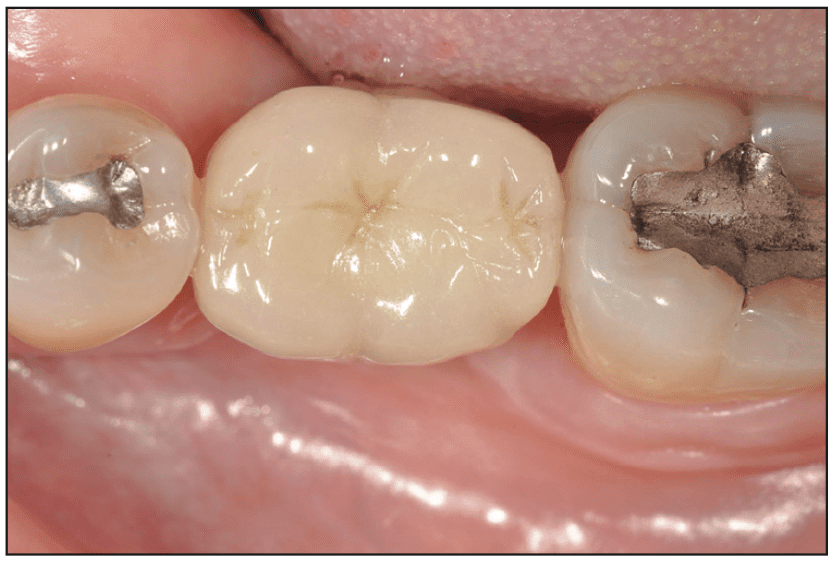
1. A No. 19 crown-abutment complex was noted to be “loose” by the patient (Figure 1).
Figure 1. Tooth No. 19 implant crown.
2. A radiograph was taken, and the implant was identified as an AstraTech Implant System/OsseoSpeed TX 3.5/4.0 implant (Dentsply Sirona Implants) using whatimplantisthat.com. The torque value was noted as 20 Ncm for the abutment screw (Figure 2).
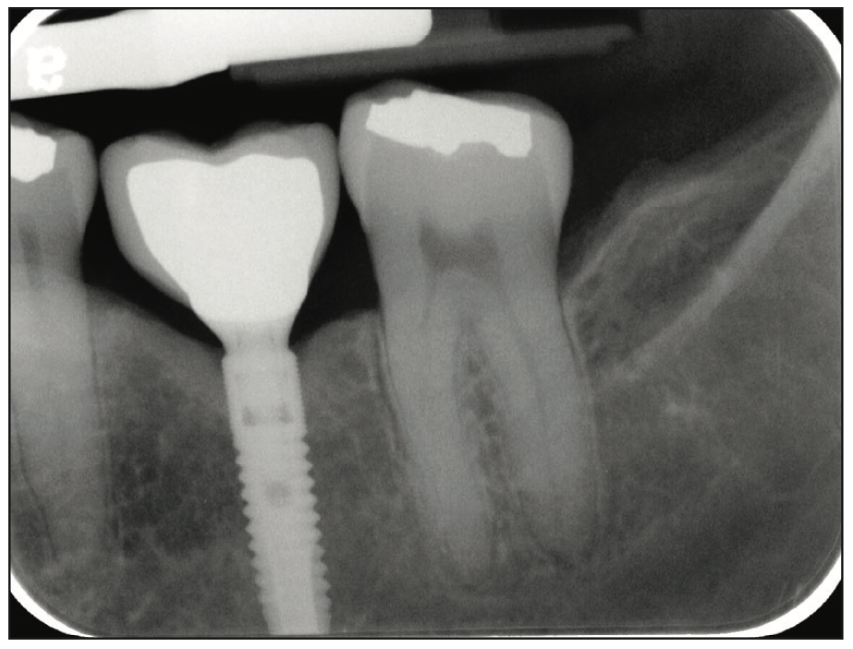
Figure 2. Tooth No. 19 implant crown radiograph.
3. Penetration of the porcelain layer of the implant crown was done with a ZR6801 018 round bur (Komet USA). The white stripe indicates that the bur is engineered for grinding all types of ceramics, including zirconia. The green stripe indicates that the “grit size” is coarse. An EVO.15 1:5L Micro-Series CoolTouch+ electric handpiece was utilized at 200,000 rpm with copious amounts of water spray to minimize potential chipping and microcracks in ceramic (Figure 3).

Figure 3. Penetration of the porcelain layer of the implant crown with a ZR6801 018 round bur (Komet USA).
4. Penetration of the metal substructure was done using an H34 012 bur (Komet USA) that is designed for cutting metal and is very good at removing metal crowns. It was used at 200,000 rpm (Figure 4).

Figure 4. Penetration of the metal substructure of the implant crown with an H34 012 metal crown remover bur (Komet USA).
5. The screw access chimney appeared to have Cavit internally. Cavit was received with a 6SE latch grip (Komet) with an electric slow-speed contra-angle EVO.15 1:1L Micro-Series handpiece utilized at 20,000 rpm. The cotton pellet below the Cavit was removed to expose the head of the abutment screw (Figure 5).

Figure 5. Removal of Cavit over a cotton pellet with an 6SE slow speed round bur (Komet USA).
6. An AstraTech hexagonal screwdriver was used to loosen the abutment screw and remove the crown-abutment complex. The AstraTech Implant System/OsseoSpeed TX implant was inspected internally to verify that there was no fracture of the implant or stripping of the internal hexagon (Figure 6).
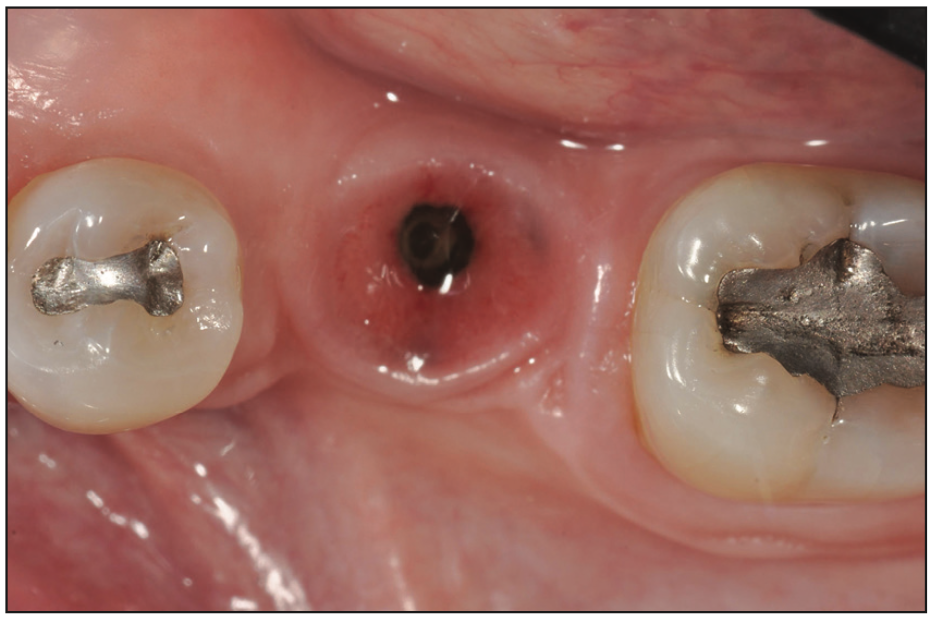
Figure 6. Inspection of the implant fixture and internal hexagon.
7. Initially in this case, the screw was unable to be removed from the crown-abutment complex. The chimney of the crown-abutment complex was reamed with an 851 016 round end bur (Komet USA) tapered with a safety tip to avoid damage to the head of the abutment screw. The key point is to hold the crown-abutment complex such that the abutment screw is held down and will not contact the 851 016 bur. Clinicians may elect to attach the crown-abutment complex to a laboratory analog at this step to act as a “handle” and prevent the abutment screw from being damaged (Figure 7).
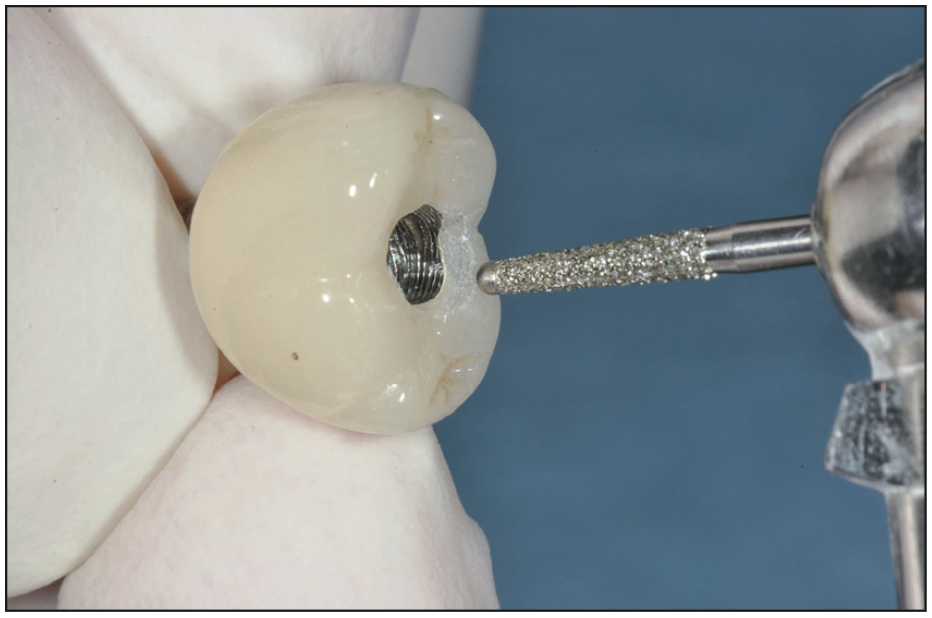
Figure 7. Reaming of the screw access chimney of the implant crown and abutment with an 851 016 round end tapered bur with a safety tip (Komet USA).
8. Inspect the screw and abutment hexagon for damage. If either is stripped or worn, replacement is necessary (Figure 8).
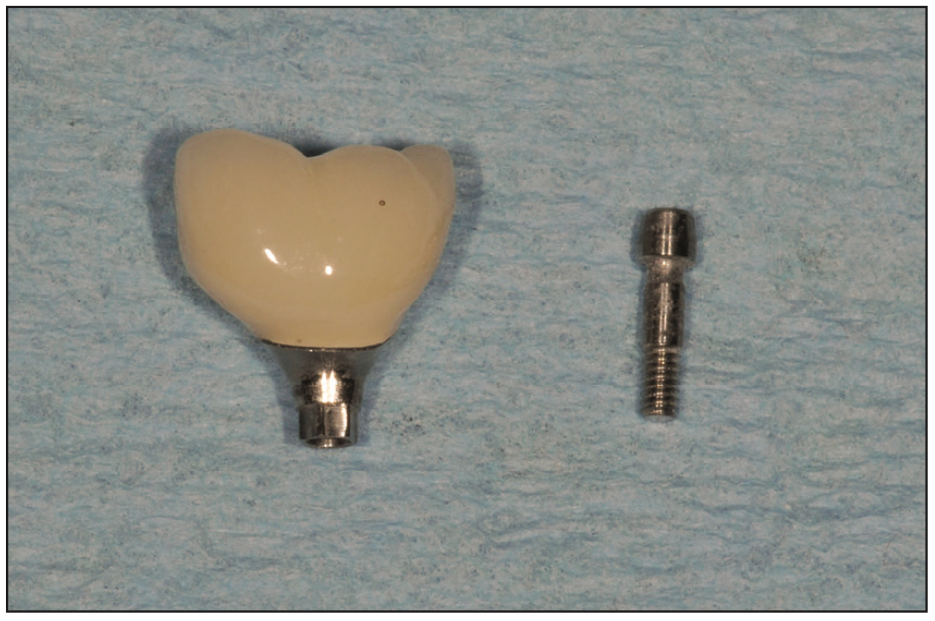
Figure 8. Inspection of the abutment screw and abutment hexagon.
9. The abutment screw was tightened to 20 Ncm of torque. The seating of the crown-abutment complex was verified with a radiograph. The prosthetic screw was covered with polytetrafluorethylene tape, commonly known as Teflon tape, plumber’s tape, or TFE (tetrafluoroethylene) threaded seal tape (Oatey Co). The access was sealed with composite (Filtek Z250 Universal Restorative [3M]) and cured for 20 seconds using a curing light (Parkell curing light [Parkell]). Occlusion was confirmed, and the patient was dismissed (Figure 9).

Figure 9. The tooth No. 19 recommissioned crown-abutment complex with the screw access sealed with PTFE tape and composite.
CONCLUSION
As mentioned, the most common complication for single implant crowns is screw loosening, which occurs at a frequency of 3%. It is important that a loose abutment screw not be ignored but dealt with immediately to prevent irreversible damage to the crown-abutment complex or the implant. The use of appropriate instrumentation, including burs and handpieces, is necessary to prevent damaging the crown-abutment complex so it can be recommissioned into a screw-retained restoration.
REFERENCES
1. Moraschini V, Poubel LA, Ferreira VF, et al. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015;44(3):377–88. doi:10.1016/j.ijom.2014.10.023
2. Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009;80(9):1388–92. doi:10.1902/jop.2009.090115
3. Hess TA. A technique to eliminate subgingival cement adhesion to implant abutments by using polytetrafluoroethylene tape. J Prosthet Dent. 2014;112(2):365–8. doi:10.1016/j.prosdent.2013.06.026
4. Wadhwani C, Rapoport D, La Rosa S, et al. Radiographic detection and characteristic patterns of residual excess cement associated with cement-retained implant restorations: a clinical report. J Prosthet Dent. 2012;107(3):151–7. doi:10.1016/S0022-3913(12)60046-8
5. Wadhwani C, Hess T, Piñeyro A, et al. Cement application techniques in luting implant-supported crowns: a quantitative and qualitative survey. Int J Oral Maxillofac Implants. 2012;27(4):859–64.
6. Wadhwani C, Piñeyro A, Hess T, et al. Effect of implant abutment modification on the extrusion of excess cement at the crown-abutment margin for cement-retained implant restorations. Int J Oral Maxillofac Implants. 2011;26(6):1241–6.
7. Wadhwani C, Hess T, Faber T, et al. A descriptive study of the radiographic density of implant restorative cements. J Prosthet Dent. 2010;103(5):295-302. doi:10.1016/S0022-3913(10)60062-5
8. Goodacre BJ, Goodacre SE, Goodacre CJ. Prosthetic complications with implant prostheses (2001-2017). Eur J Oral Implantol. 2018;11(Suppl 1):S27-S36.
9. Goodacre CJ, Bernal G, Rungcharassaeng K, et al. Clinical complications in fixed prosthodontics. J Prosthet Dent. 2003;90(1):31-41. doi:10.1016/s0022-3913(03)00214-2
10. Hess TA. The Tucker technique: the proximal hollow grind to address a root concavity. Oper Dent. 2014;39(5):454–9. doi:10.2341/13-158-T
11. Hess TA, Wadhwani CP. The Tucker technique: conservative molar inlays preserving the transverse ridge. Oper Dent. 2012;37(1):93–7. doi:10.2341/11-048-T
12. Pereira GKR, Fraga S, Montagner AF, et al. The effect of grinding on the mechanical behavior of Y-TZP ceramics: A systematic review and meta-analyses. J Mech Behav Biomed Mater. 2016;63:417–42. doi:10.1016/j.jmbbm.2016.06.028
13. McGlumphy EA, Papazoglou E, Riley RL. The combination implant crown: a cement- and screw-retained restoration. Compendium. 1992;13(1):34, 36, 38 passim.
ABOUT THE AUTHOR
Dr. Hess is a graduate of the University of Alberta and completed his DDS degree from the University of Washington (UW) in 1994. He is an affiliate assistant professor of restorative dentistry, an affiliate assistant professor of oral medicine, and the director of the Tucker Institute at the UW School of Dentistry. He is director of education at the Washington Academy of General Dentistry Global Learning Center. Dr. Hess lectures nationally and internationally and has published articles in numerous peer-reviewed journals. He is a member of the International Academy of Gnathology and an active member of the American Academy of Restorative Dentistry. He can be reached at drhess@tahessdds.com.
Disclosure: Dr. Hess reports no disclosures.